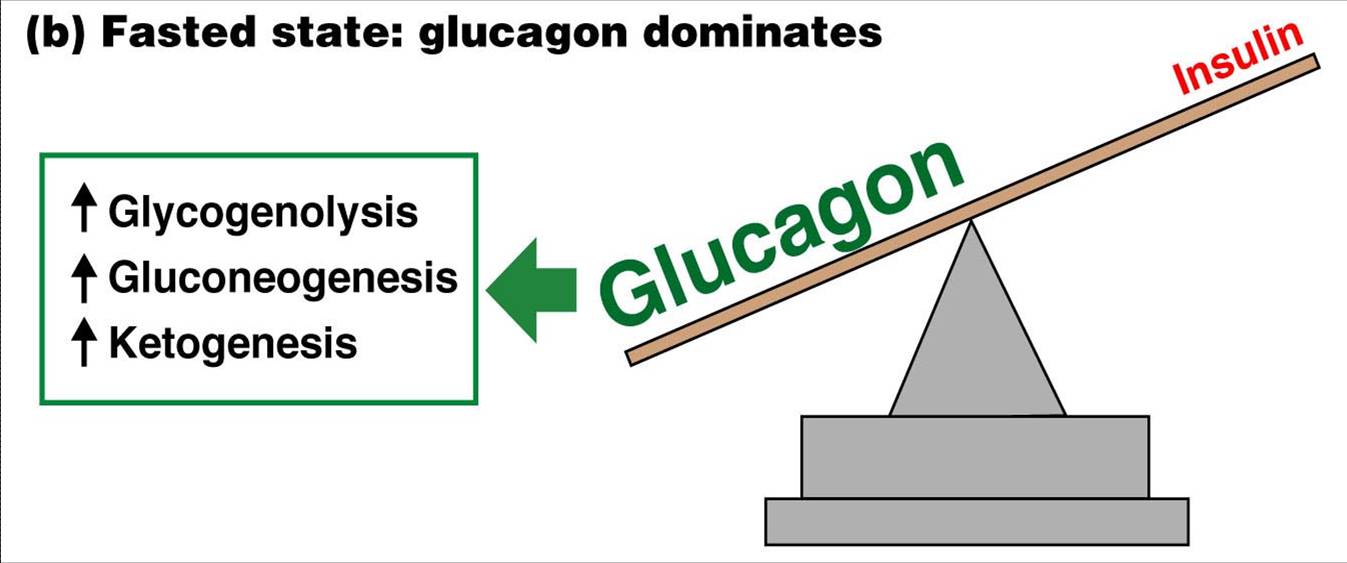
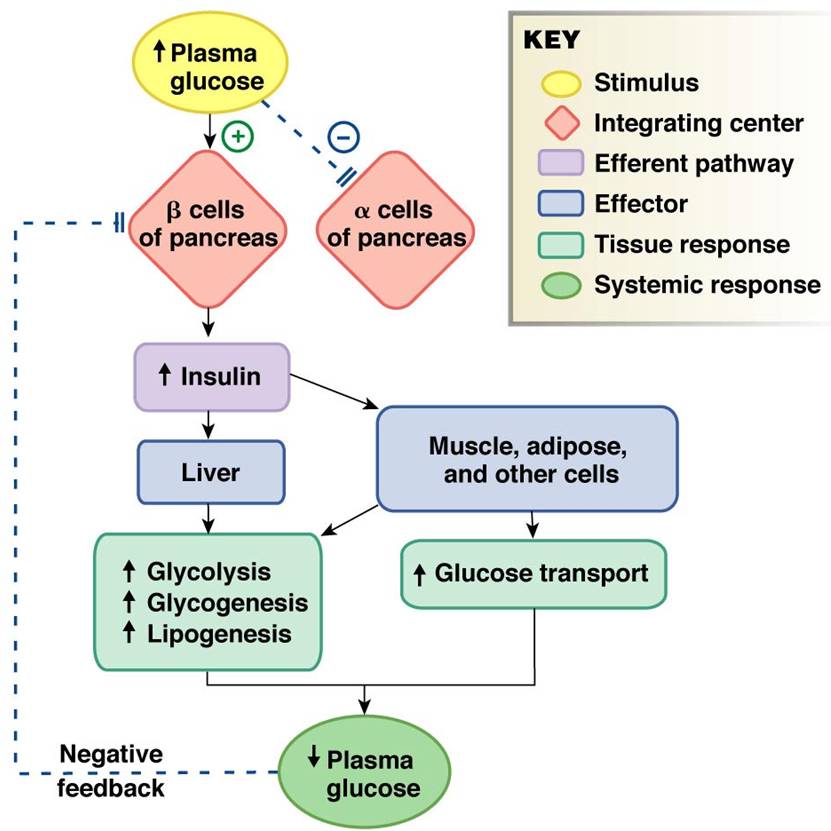
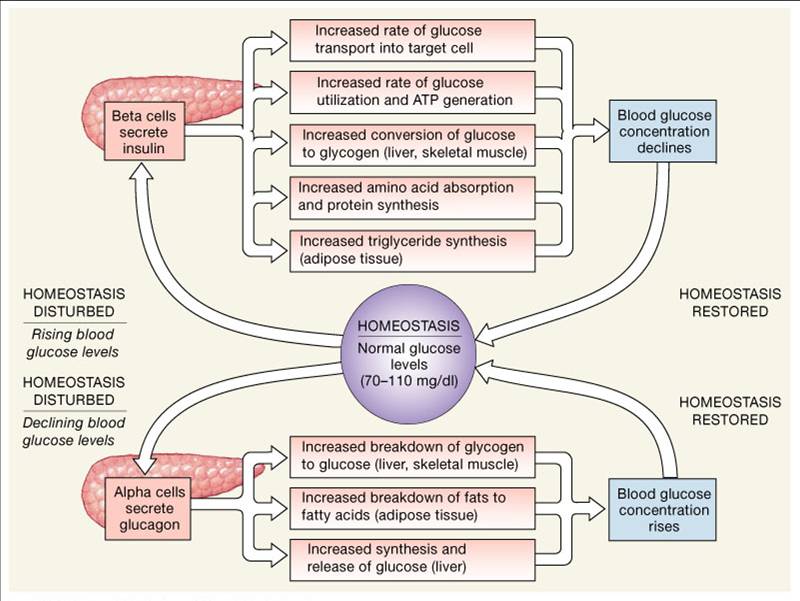
Glucagon raises blood glucose by increasing the rates of glycogen breakdown and glucose manufacture by the liver
Glucose regulation and metabolism terms:
- Gluconeogenesis - Synthesis of glucose from noncarbohydrate precursors,
Lactic acid, glycerol, amino acids, liver cells synthesis glucose when carbohydrates are depleted
- Glycogenesis - Formation of glycogen, glucose stored in liver and skeletal muscle as glycogen, important energy reserve
- Glycogenolysis – breakdown of glycogen (polysaccharide) into glucose molecules (monosaccharide)
- Glycolysis - the breakdown of glucose into pyruvate by cells for the production of ATP
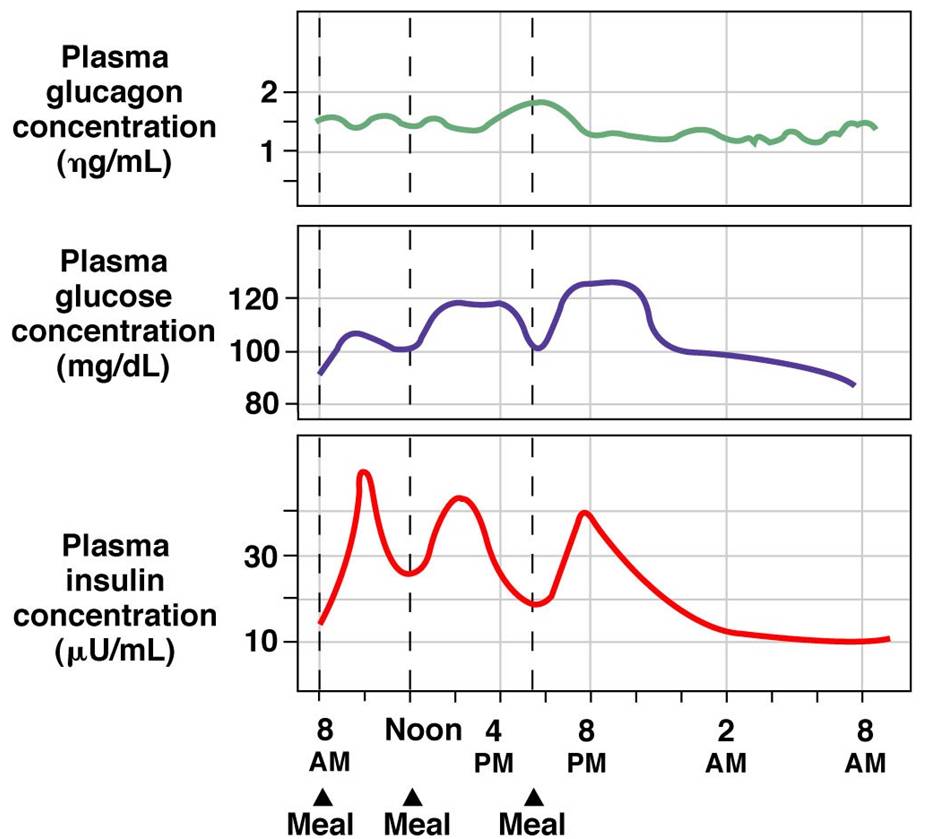
Blood Glucose Regulation - Glucose, glucagon, and insulin levels over a 24-hour period
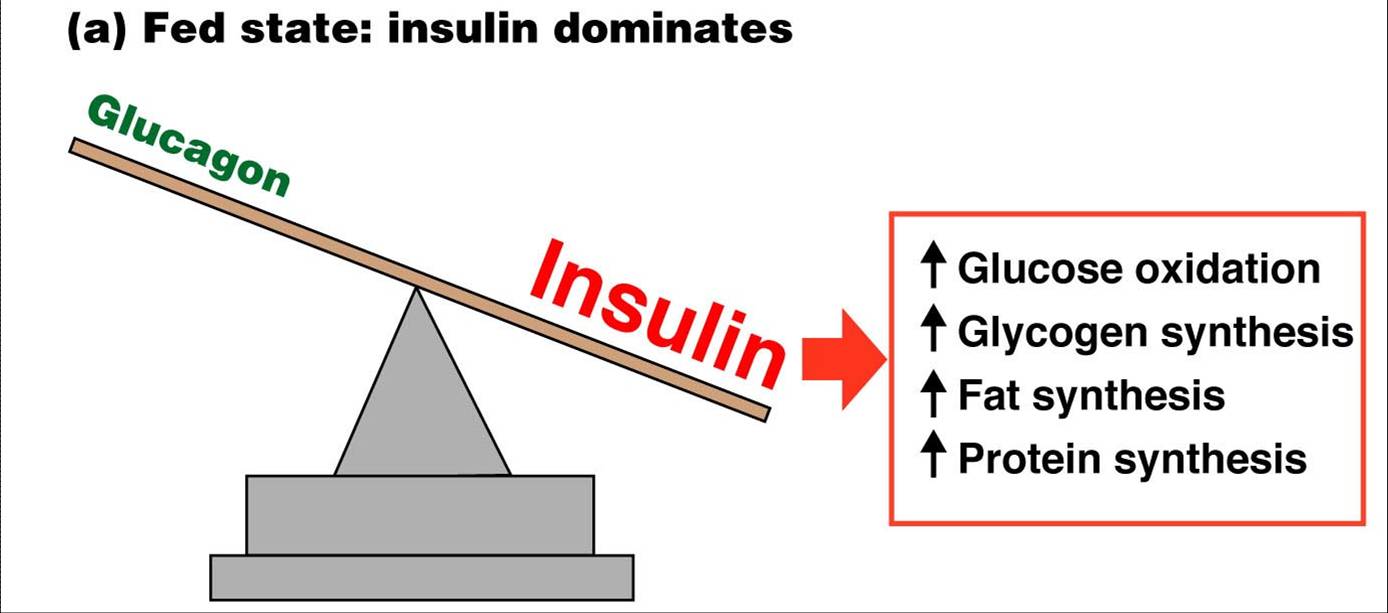
Insulin - Glucagon Summary

Fed-state metabolism under the influence of insulin promotes glucose metabolism by cells
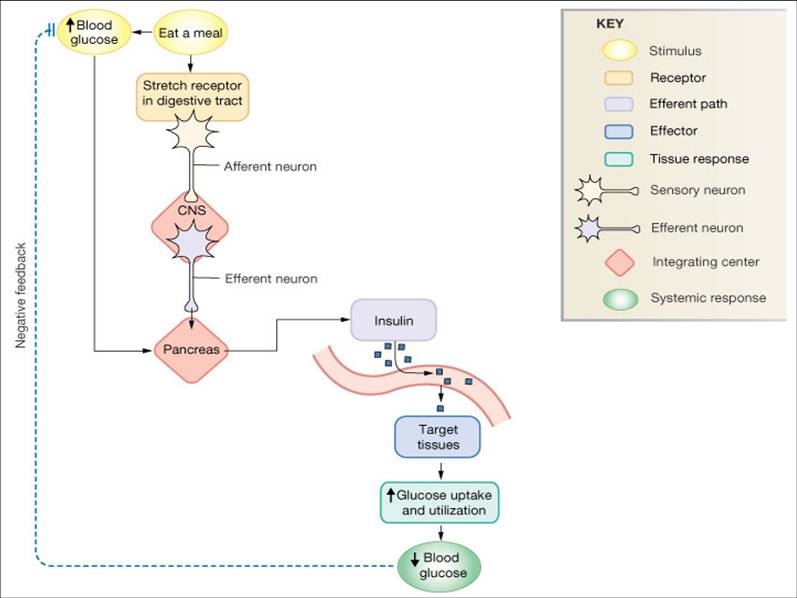
Stimuli for Insulin Secretion
- Increased glucose concentrations
- Increased amino acids concentrations
- Feedforward effects of GI hormones
Multiple Stimuli for Insulin Release
Endocrine Response to Hypoglycemia

Insulin Action
- Increases glucose transport into most, but not all, insulin-sensitive cells
- Enhances cellular utilization and storage of glucose
- Enhances utilization of amino acids
- Promotes fat synthesis
In the absence of insulin, glucose cannot enter the cell
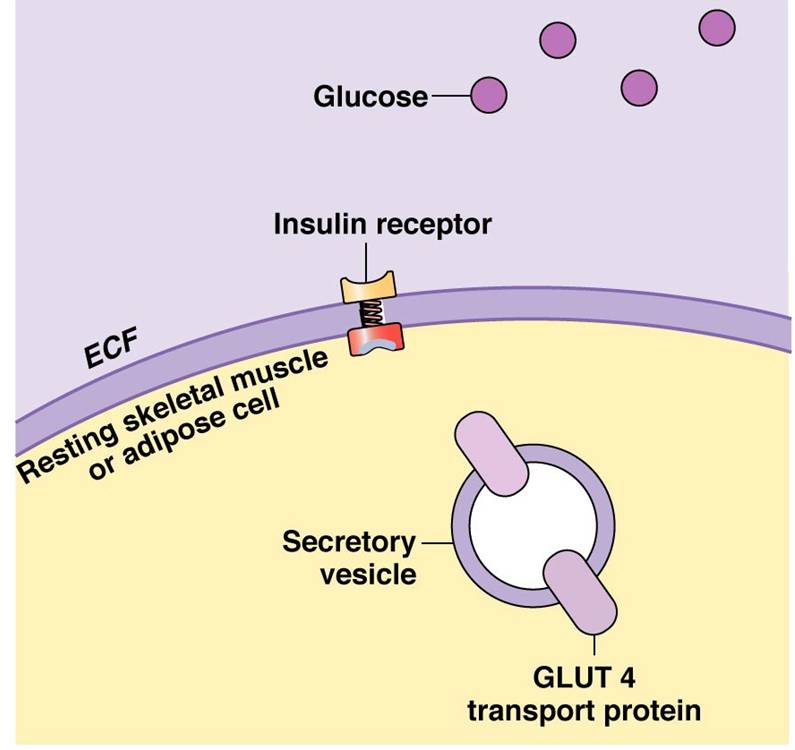
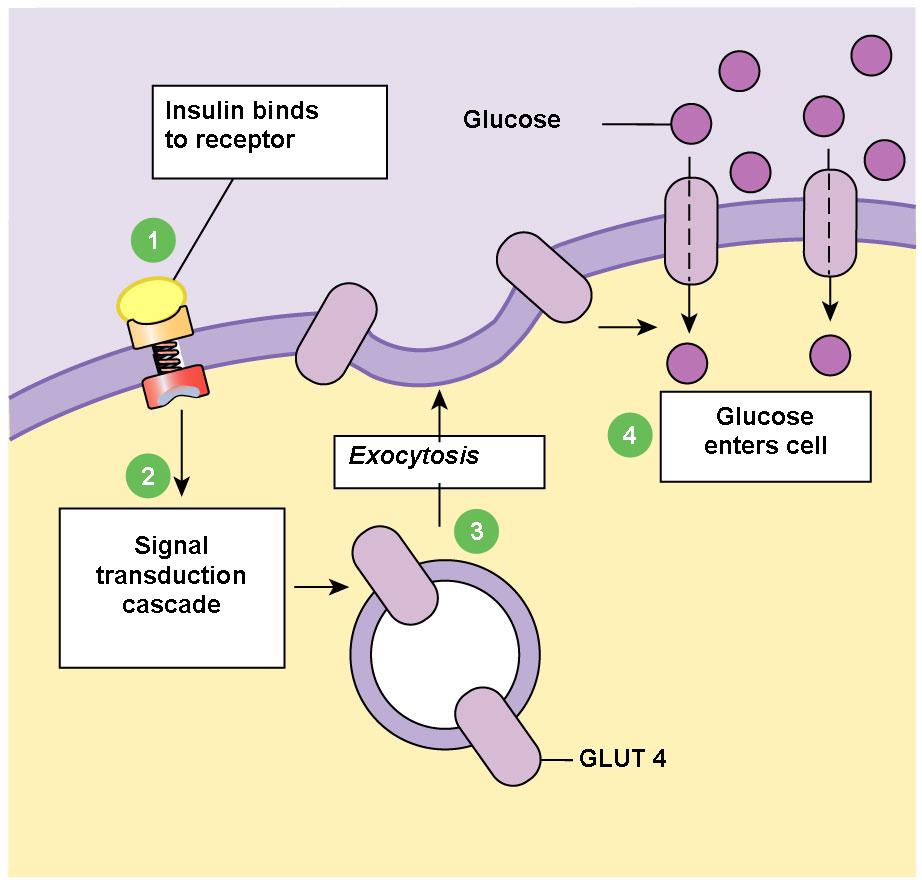
Insulin enables glucose uptake by adipose tissue and resting skeletal muscle
Insulin binds to receptor, initiates the synthesis of glucose transporters (GLUT 4) the GLUT 4 transpor proteins are integrated into the cell membrane allowing glucose to be transported into the cell
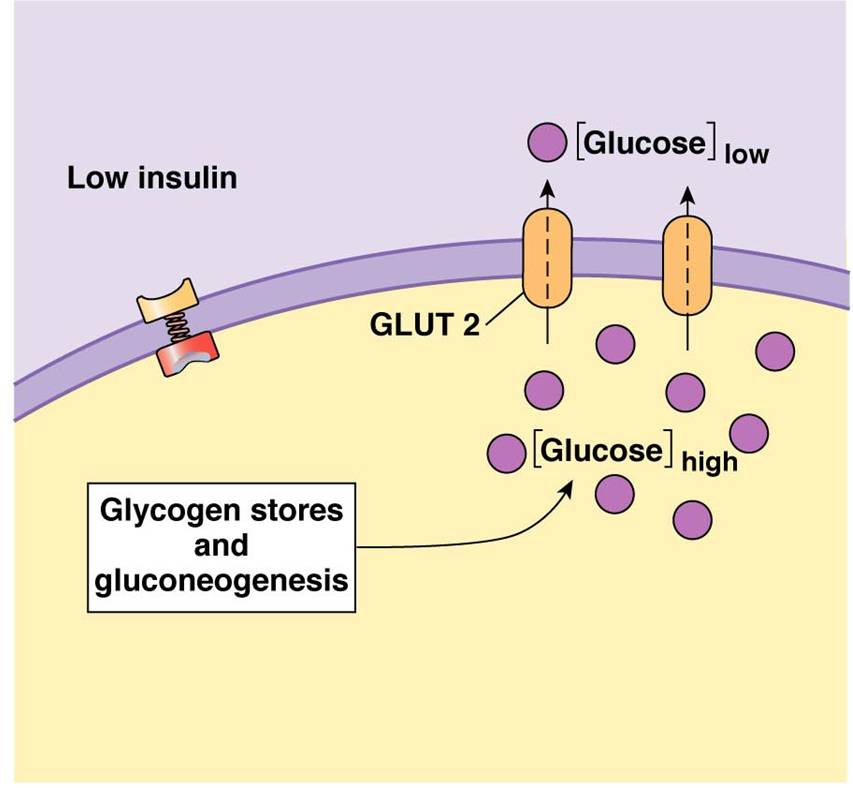
Insulin acts indirectly to alter glucose uptake in hepatocytes: in fed state liver cells take up glucose

A hepatocyte in the fasted state makes glucose and transports it out into the blood
Regulation of Blood Glucose Concentrations
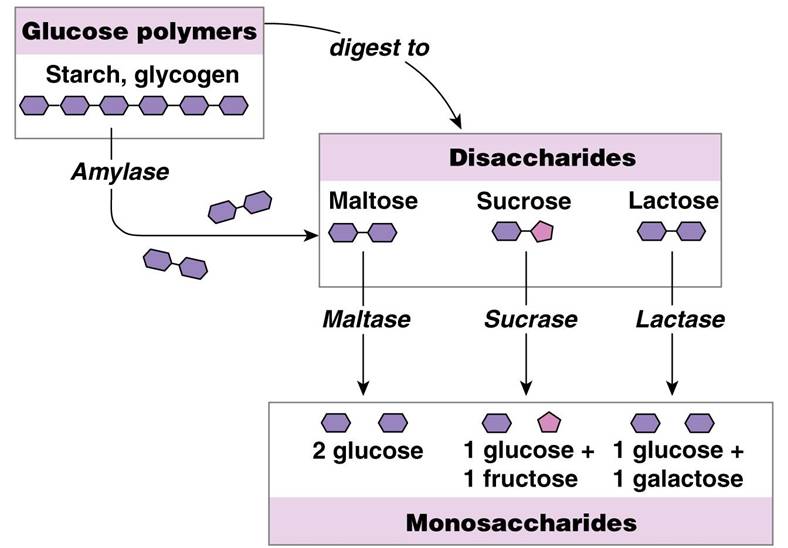
Chemical Digestion: Carbohydrates
- Salivary and pancreatic enzymes catabolize into disaccharides and trisaccharides
- Brush border cells of the small intestine release enzymes to further catabolize into monosaccharides
- Absorption of monosaccharides occurs across the intestinal epithelia
- Enzymes used: salivary amylase, pancreatic amylase, and brush border enzymes
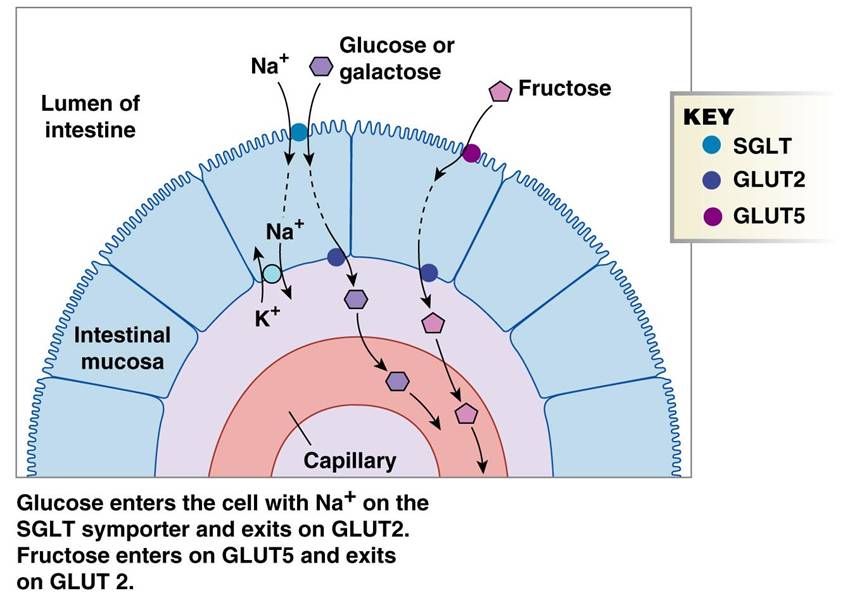
Carbohydrate Absorption in the Small Intestine:
Absorption: via cotransport with Na+, and facilitated diffusion
Enter the capillary bed in the villi
Transported to the liver via the hepatic portal vein
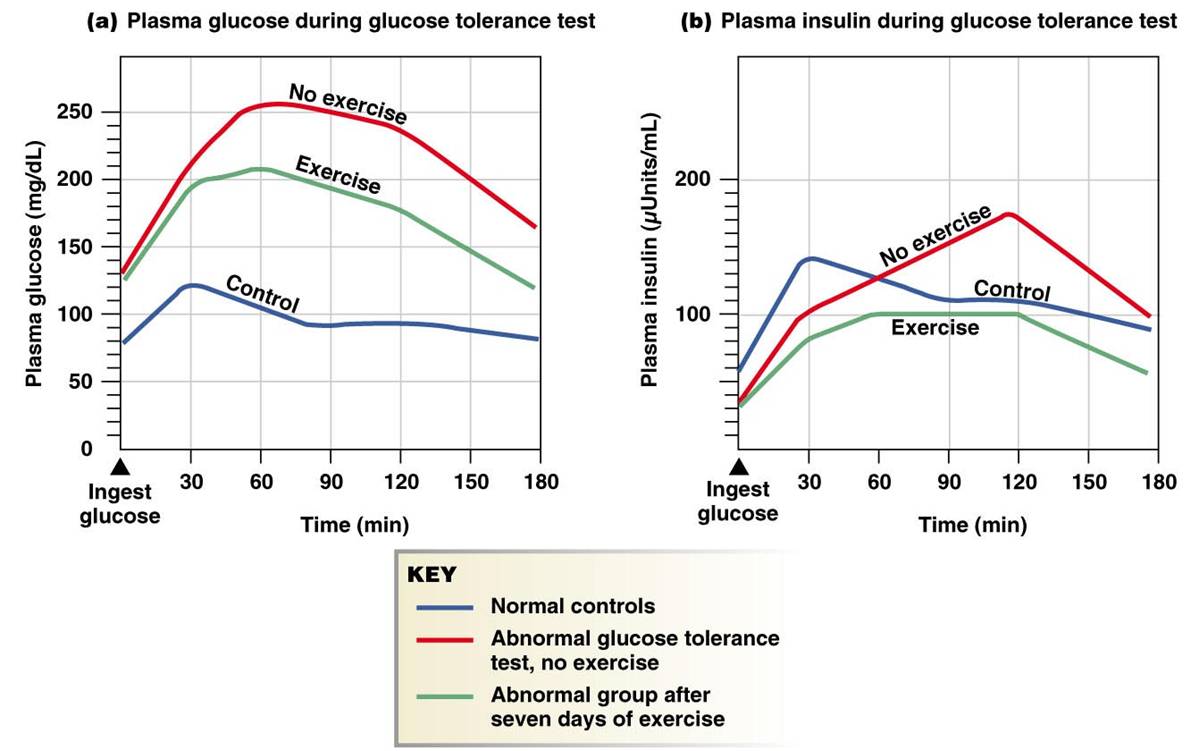
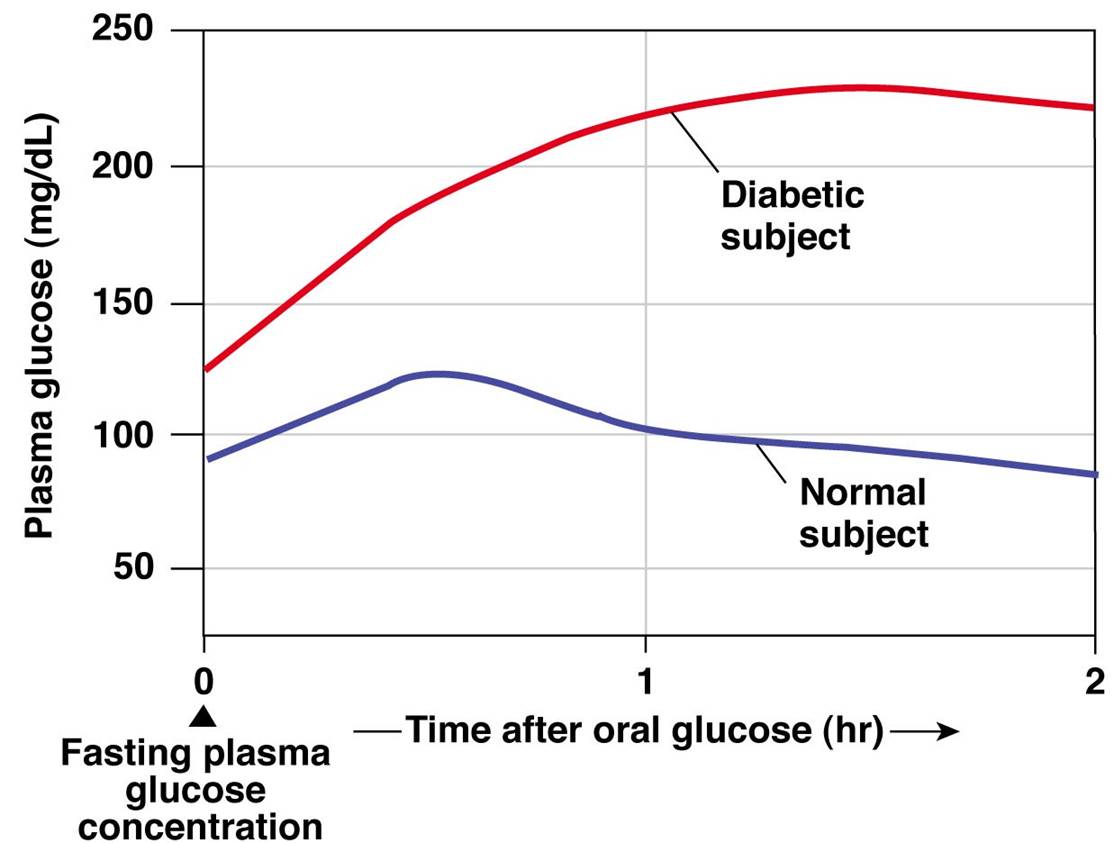
Normal and Abnormal Results of Glucose Tolerance Tests
Renal Reabsorption of Glucose
- Na+ linked secondary active transport
- Key site - proximal convoluted tubule (PCT)
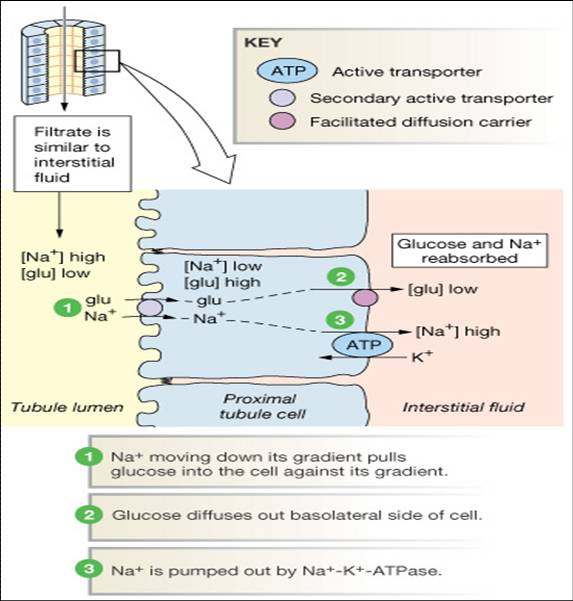
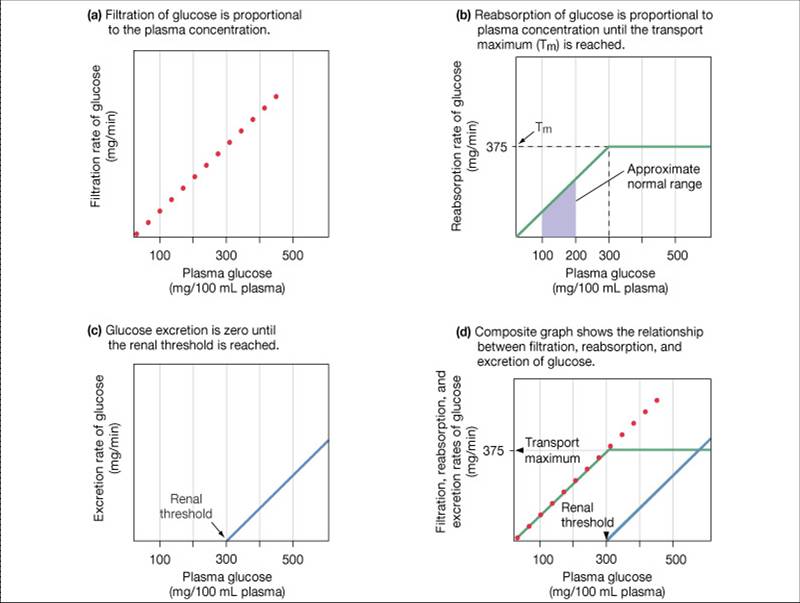
Reabsorption: Transport Maximum
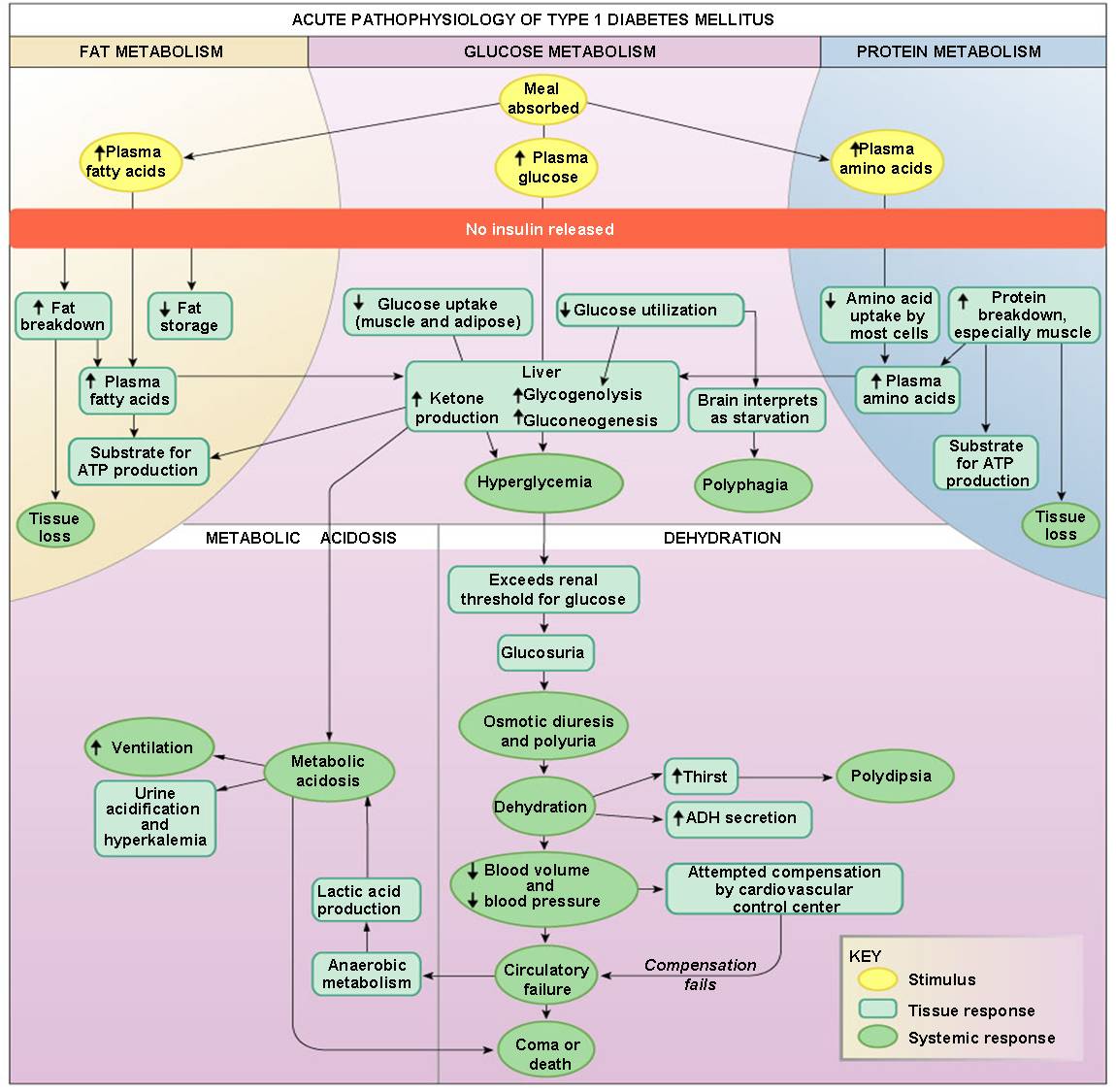
Type 1 diabetes mellitus is characterized by loss of the insulin-producing beta cells of the islets of Langerhans in the pancreas leading to a deficiency of insulin
Type 2 diabetes mellitus is characterized differently and is due to insulin resistance or reduced insulin sensitivity, combined with relatively reduced insulin secretion which in some cases becomes absolute. The defective responsiveness of body tissues to insulin almost certainly involves the insulin receptor in cell membranes
- Accounts for 90% of all diabetics
- Complications include atherosclerosis, neurological changes, renal failure, and blindness
- Therapy
Regulation of Glucose Metabolism During Exercise
- Glucagon secretion increases during exercise to promote liver glycogen breakdown (glycogenolysis)
- Epinephrine and Norepinephrine further increase glycogenolysis
- Cortisol levels also increase during exercise for protein catabolism for later gluconeogenesis.
- Thyroxine promotes glucose catabolism
As intensity of exercise increases, so does the rate of catecholamine release for glycogenolysis
During endurance events the rate of glucose release very closely matches the muscles need
When glucose levels become depleted, glucagon and cortisol levels rise significantly to enhance gluconeogenesis.
Glucose must not only be delivered to the cells, it must also be taken up by them. That job relies on insulin.
Exercise may enhance insulin’s binding to receptors on the muscle fiber.
Up-regulation (receptors) occurs with insulin after 4 weeks of exercise to increase its sensitivity (diabetic importance).
The effects of exercise on glucose tolerance and insulin secretion