Integumentary System
|
Content
Integumentary System
Structures/Layers of the Skin
Skin Color
Sebaceous Glands
Sweat Glands
Mammary Glands
Ceruminous Glands
Skin Injury and Repair
Nails
Hair
Integumentary System
The skin and its associated structures (hair, nails, sweat glands, and oil glands) make up a complex body system called the integumentary system.

Functions of the Integumentary System
The integumentary system has many functions:
- Protects Against
- invasion of microorganisms
- UV damage
- mechanical damage
- It also contains macrophages, lymph nodes and other structures which identify pathogens and provide first line of defense against the
- Prevents Water Loss
- The epidermis is water resistant and prevents unnecessary water loss.
- Regulates Body Temperature
- By diverting blood into or away from the skin the body can release or conserve heat.
- The skin can also release sweat which releases heat when the water in the sweat evaporates off of the skin
- Regulates Calcium and Phosphate Levels
- Certain cells in the skin use the UV rays that penetrate the skin to synthesize (make) cholecalciferol
- The cholecalciferol goes to the kidneys where it is converted to calcitriol, which is a hormone that is the active form of Vitamin D3. Vitamin D3 helps the body absorb calcium and phosphate from the food we eat (this is done in the small intestine). All you need is 15 minutes of sun a day to get your vitamin D requirement.
- Defends Against Pathogens
- The skin contains cells called epidermal dendritic cells or Langerhan cells that can phagocytize pathogens that have penetrated the skin and also epidermal cancer cells.
- Allows Sensations
- The skin contains sense organs for light touch, pressure, temperature, and pain.
- Excretes Substances
- Skin excretes sweat and sebum (which contain substances including water, urea and salts).
- In females, the skin also produces milk
Structure of the Skin
The skin consists of two parts:
1. Epidermis (outer layer)
2. Dermis (inner layer)
Beneath the dermis lies the subcutaneous layer also known as the hypodermis or superficial fascia.

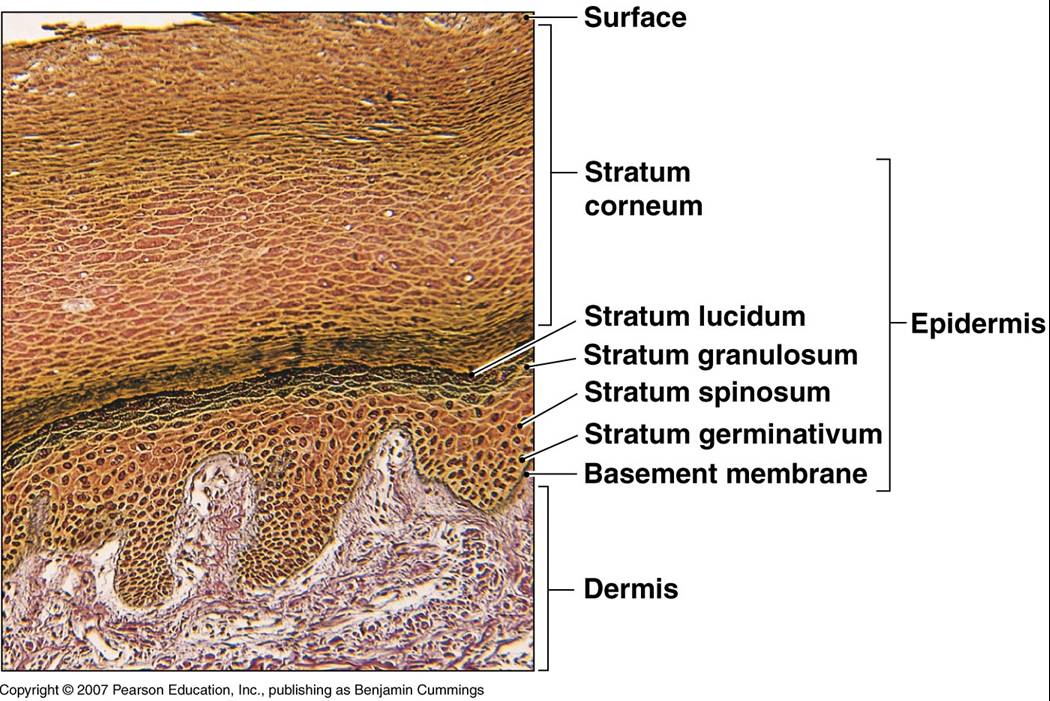
Epidermis
- Is avascular
- Is made of stratified squamous epithelium divided into 5 sublayers:
- Stratum Basale - basal layer, single row of cells
- When a basal layer cell divides, one daughter cell migrates through the different layers to the surface where its nucleus degenerates and the cytoplasm fills with a tough waterproof protein called keratin.
- The cell then dies, becomes flat, and eventually shed.
- Stratum Spinosum - spiny layer, 8 to 10 rows
- Stratum Granulosum - granular layer, 3-5 rows, keratin visible
- Stratum Lucidum - clear layer, transparent keratin called eleiden, absent on hairy skin, found on palms, soles
- Stratum Corneum - horny skin, 25 to 30 rows, keratinized, flat, dead.
|
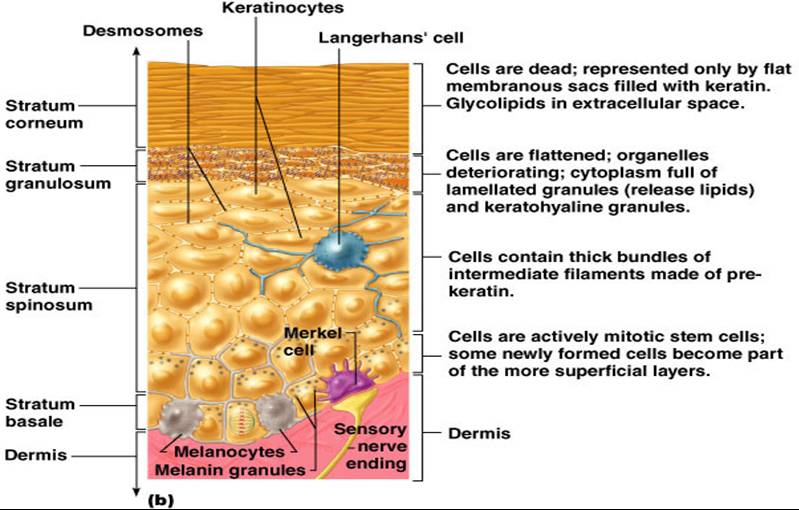
Epidermal Cells
The epidermis is made up of several different types of cells
- Keratinocytes
- 90% of epidermal cells are keratinocytes
- Produce keratin
- Have anchoring junctions called desmosomes that act as spot welds
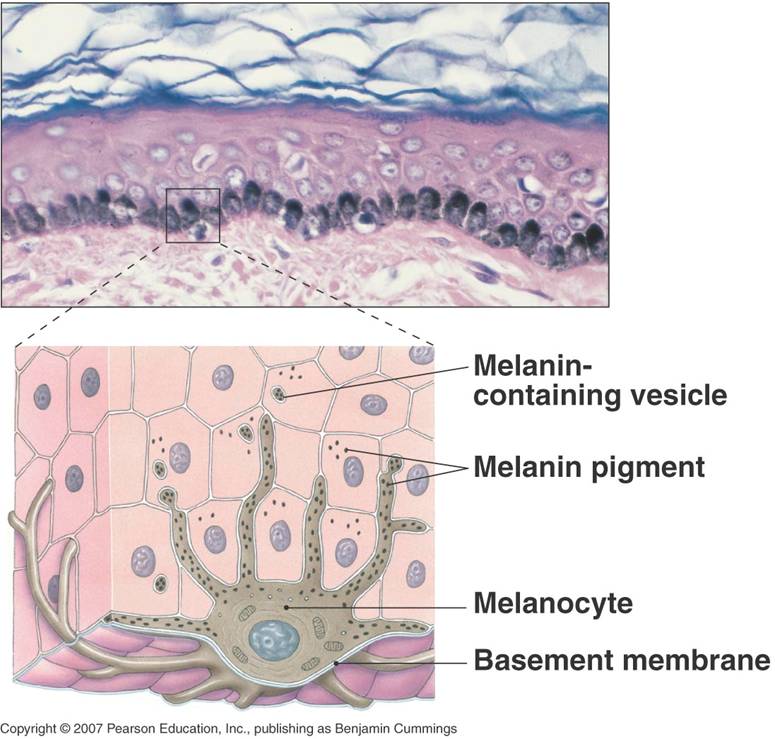
- Melanocytes
- 8% of epidermal cells are melanocytes
- Produce the pigment melanin which absorbs UV light thereby protecting cell nuclei (DNA)
- Melanin varies in color from yellow to reddish to brown to black.
- Differences in skin color occur because of variations in :
- Melanin color
- Number of melanin granules in a person's skin
- Amount of pigment in each melanocyte
- Langerhans Cells
- Migrate from bone marrow involved in immunity by assisting helper T cells
- Merkel Cells
- Make contact with flattened sensory nerve endings (merkel discs), function in touch sensation.
|
Dermis
- Made of connective tissues
- Cells include fibroblasts, macrophages, and adipocytes (fat cells)
- Has nerve endings, capillaries, muscles, glands, and hair follicles
- It assists in the production of the active form of vitamin D (calcitriol) using UV light. Vitamin D helps in the absorption of calcium from foods
- Made of 2 sublayers:
- Papillary Layer
- made of areolar connective tissue
- it is folded into numerous dermal papillae, which increase surface area and prevent the skin from sliding and shifting
- The epidermis conforms to the papillae creating epidermal ridges (fingerprints)
- Reticular layer
- Is the deeper layer
- Is made of of dense irregular connective tissue which provides strength, elasticity and extensibility
|
Hypodermis (also called Subcutaneous Layer or Superficial Fascia)
- Is the layer deep to the skin
- Is made of adipose and areolar connective tissue
- Is not considered part of the skin
Skin Color
Three pigments contribute to skin color:
1. Melanin
- Uellow to reddish-brown to black pigment
- Responsible for dark skin color
- Rreckles and pigmented moles result from local accumulations of melanin
2. Carotene
- Yellow to orange pigment that the body obtains from vegetable sources such as carrots and tomatoes
- most obvious in the palms and soles of the feet
3. Hemoglobin
- Blood with lots of oxygen is bright red, so the blood vessels in the dermis give the skin a reddish tint
- This is easy to see in lightly pigmented individuals
- Because Caucasian skin contains little melanin, the epidermis is nearly transparent and allows the color of blood to show through
Accessory Structures of the Skin
The skin holds many structures and derivatives:
- Nerve receptors for cold, heat, and pain, lamellated corpuscles (pressure) and corpuscles of touch
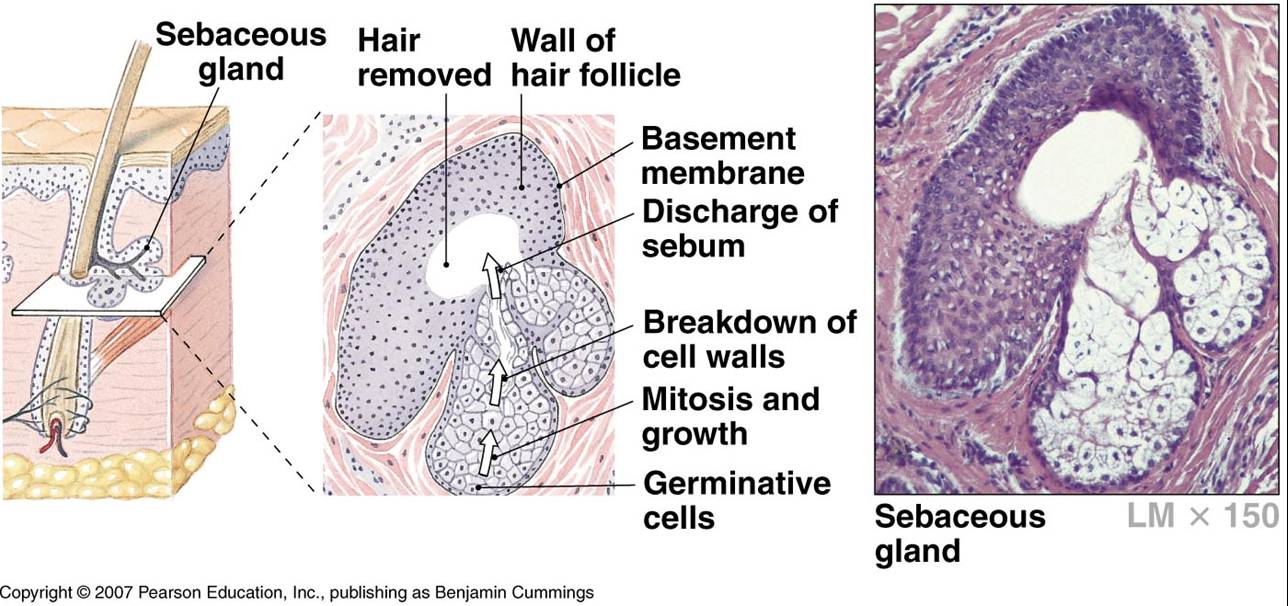
- Sebaceous (Oil) Glands
- Sudoriferous (Sweat) Glands
- Mammary Glands
- Ceruminous Glands
- Hair
- Nails
All of the above glands are made of specialized glandular (secretory) epithlelium
Sebaceous Glands
- Secrete lipid-rich sebum (oil) for waterproofing and softening of skin and hair.
Sudoriferous Glands - sweat glands
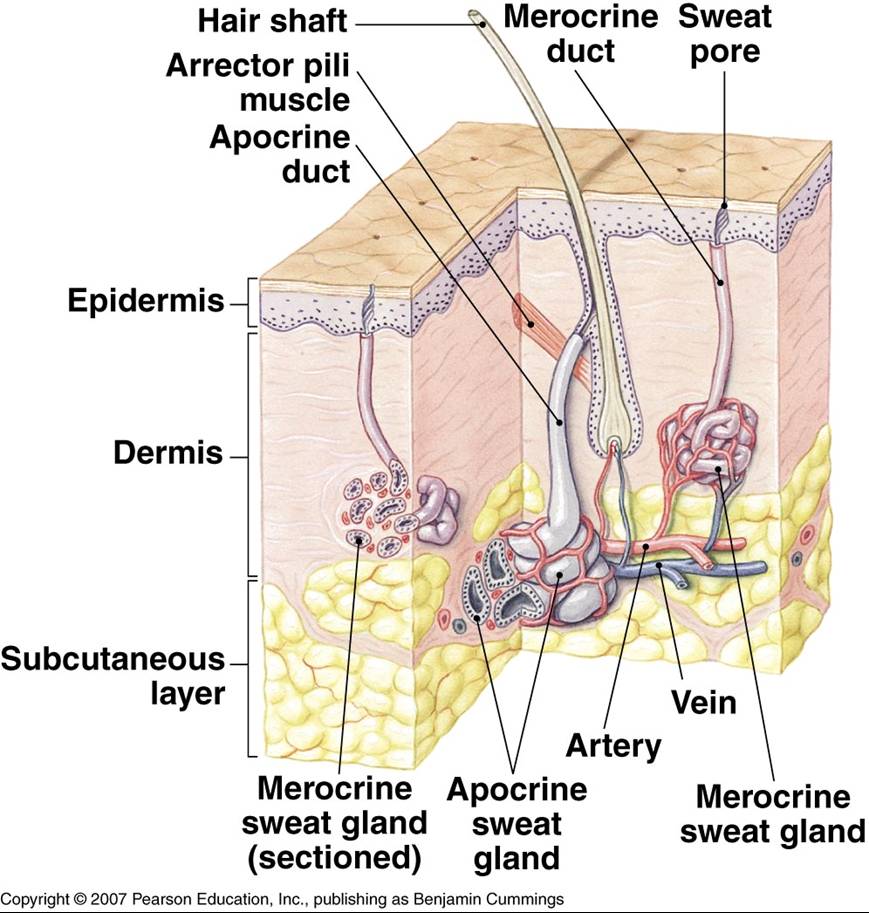
2 Types of Sweat Glands:
- Eccrine Glands
- for evaporative cooling distributed throughout the skin except margin of lips, nail beds and, genitalia
- The duct of the eccrine gland empties out on the skin surface (pores)
- Apocrine Glands
- are found in the axilla (armpit), pubic region, and areolae
- The excretory ducts empty into the hair follicle.
- Become active at puberty
- Apocrine secretion contains the same basic components as eccrine sweat, but it also contains fatty acids and proteins, giving the sweat a milky or yellowish color; the secretion is odorless, but bacteria on the skin decompose the fatty acids and proteins, giving it its characteristic musky odor.
Mammary Glands
Are specialized sudoriferous glands that secrete milk in females
Ceruminous Glands
secrete cerumen, a waxy substance, combined with sebum provides a sticky barrier in the external auditory meatus (ear canal) for protection against foreign bodies.
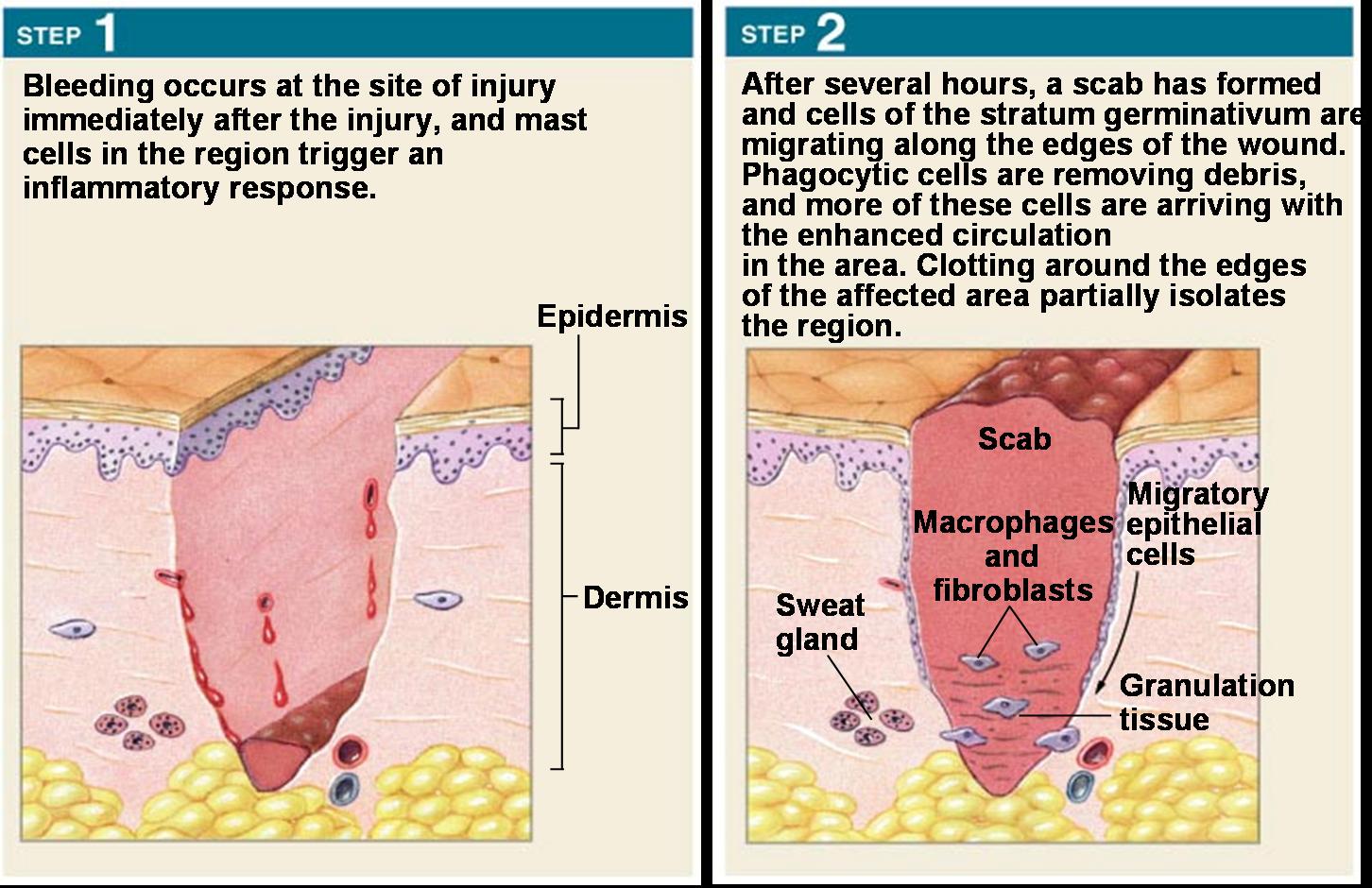
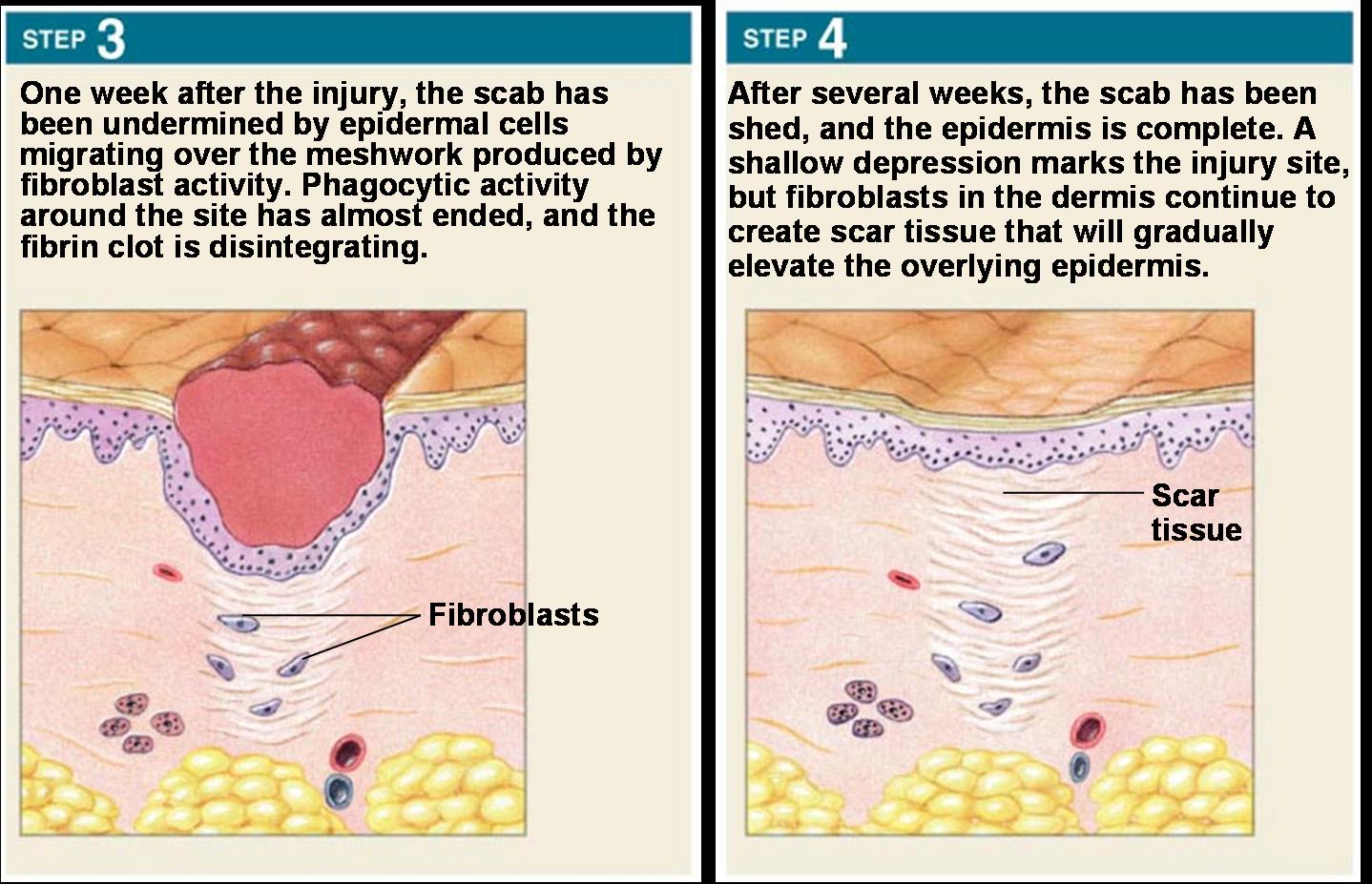
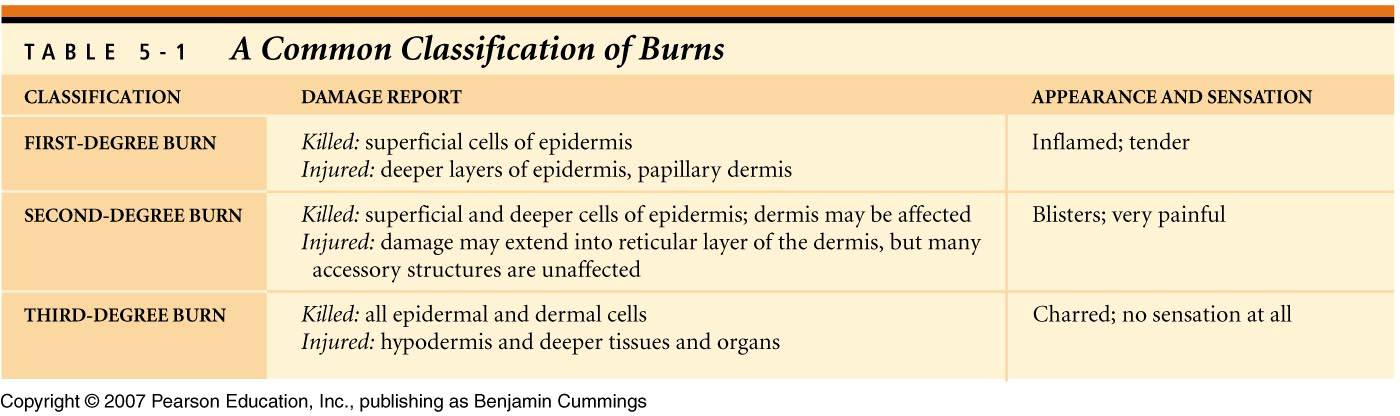
Skin Injury and Repair
Four Stages in Skin Healing:
-
Inflammation
- Blood flow increases
- Phagocytes attracted
- Scab Formation
- Cell Division and Migration
- Scar Formation
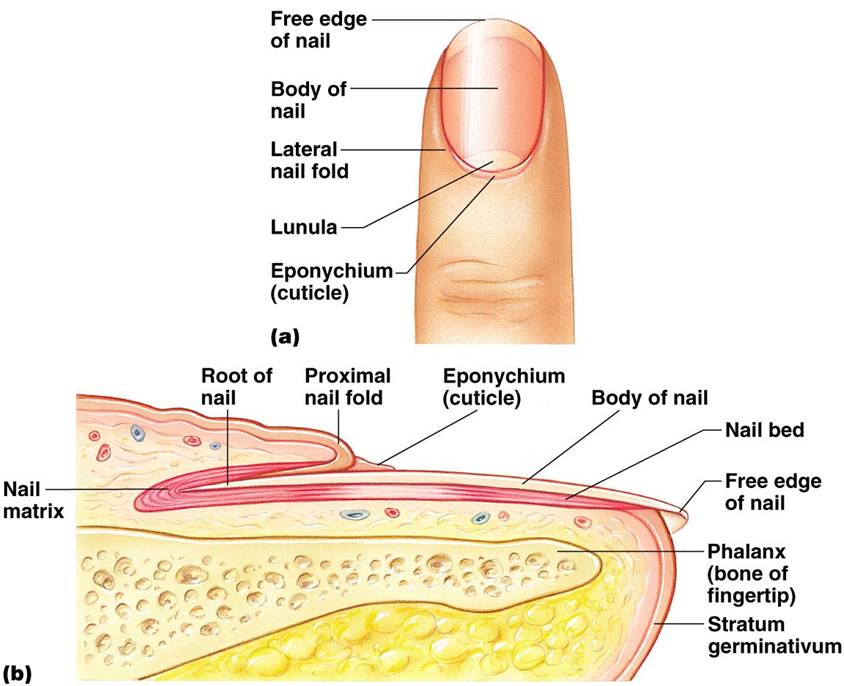
Nails
- Each nail has 3 parts; free edge, body, and nail root
- The nail does not grow from the root, but from the underlying portion of the epidermis called the nail matrix
- The cells from this area become keratinized, harden, and move forward and over the stratum germinativum (basale)
- Growth rate is approx. 1mm per week
Hair
- Is a column of dead epidermal cells covered with a layer of flattened, scale-like cells called the cuticle
- The cuticle surrounds the cortex and the central medulla which contains pigment granules and air spaces
- The part of the hair that extends from the skin surface is called the shaft
- The root is embedded in the hair follicle which is an extension of the epidermis, part of which extends into the dermis called the external root sheath
- At the base of the internal root sheath is the bulb into which a papilla protrudes
- A layer of epidermal cells called the germinal layer covers the hair papilla and gives rise to the hair itself
- Attached to the connective tissue sheath around the hair follicle is a small smooth muscle called the arrector pili
Top ....Main Page |



