Respiratory System
|
Content
Functions of the Respiratory System
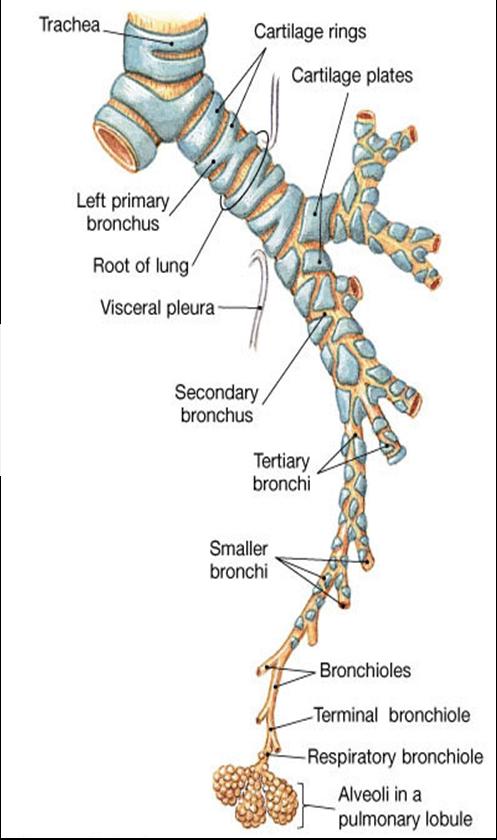
Pathway of Air
Respiratory Divisions
Respiration
Pulmonary Ventilation
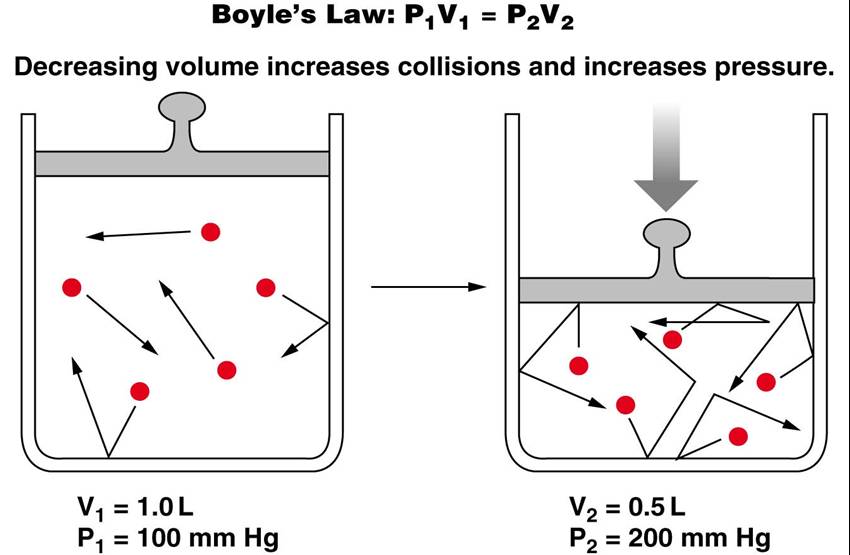
Boyle’s Law
Thoracic Volume Changes
Inspiration
Expiration
Respiratory Cycle
Airway Resistance
Gas Properties
Respiratory Membranes
Alviolar Composition
Partial Pressure Gradients
Ventilation-Perfusion
Hemoglobin Saturation
Carbon Dioxide Transport
Control of Respiration
Pons Respiratory Centers
Depth and Rate of Breathing
Functions of the Respiratory System
Breathing (Pulmonary Ventilation)
Inhalation (inspiration) draws gases into the lungs.
Exhalation (expiration) forces gases out of the lungs.
Gas Conditioning
As gases pass through the nasal cavity and paransal sinuses, inhaled air becomes turbulent. The gases in the air are
- warmed to body temperature
- humidified
- cleaned of particulate matter
Produces Sounds
The larynx, nasal cavity, paranasal sinuses, teeth, lips, and tongue work to produce sound.
Sound allows speech, singing, and nonverbal communication
Provides Olfactory Sensations
When airborne molecules are inhaled and dissolve in the mucus in the nose, the molecules can bind to receptors in the olfactory epithelium.
Protects the Body
Hairs, twisted pathways, goblet cells, mucous glands, lysozyme in the mucus all help defend the body against infection by airborne pathogens.
Pathway of Air
nose ---> pharynx ---> larynx ---> trachea ---> primary bronchi ---> secondary bronchi ---> tertiary bronchi ---> bronchioles ---> terminal bronchioles ---> respiratory bronchioles ---> alveolar duct ---> alveoli
Click here for an animation that provides an overview of the respiratory system, including its functions and organs.
|
Respiratory Divisions
- Conducting Zone
- Respiratory Zone
Conducting Zone
-
Made up of rigid passageways that serve to warm, moisten, and filter the inhaled air: nose, nasal cavity, pharynx, larynx, trachea, primary bronchi, tertiary bronchi, bronchioles, terminal bronchioles.
- Air passages undergo 23 orders of branching in the lungs which significantly increases cross sectional area for flow
|
|
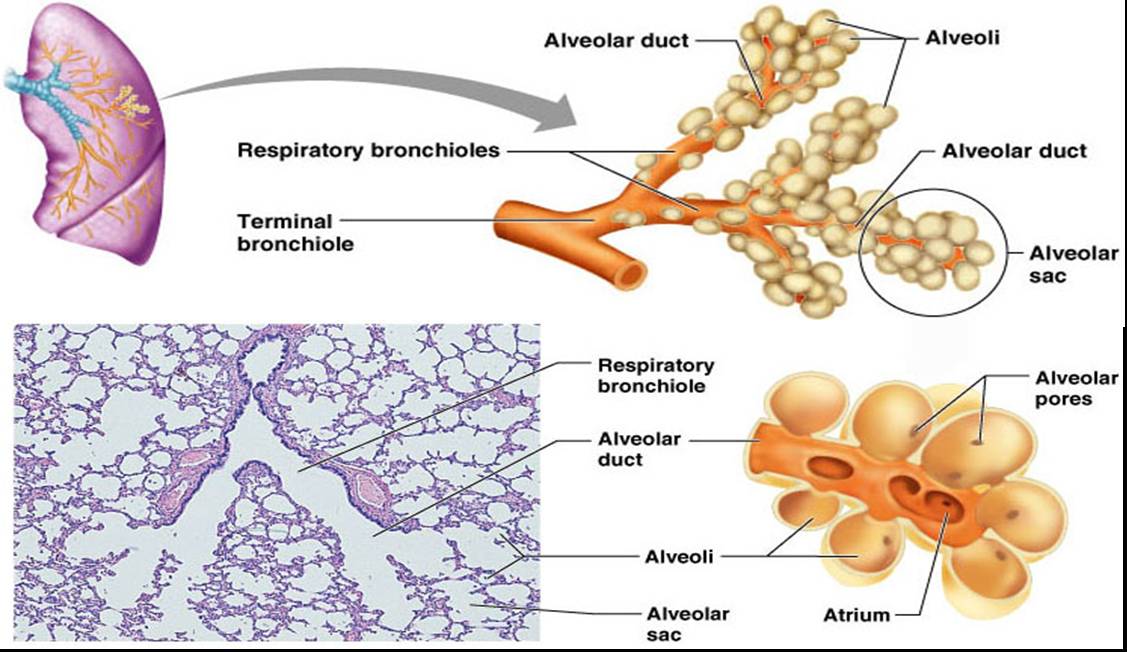
Respiratory Zone
- Site of gas exchange
- Consists of respiratory bronchioles, alveolar ducts, alveolar sacs, and about 300 million alveoli
- Accounts for most of the lungs’ volume
- Provide tremendous surface area for gas exchange
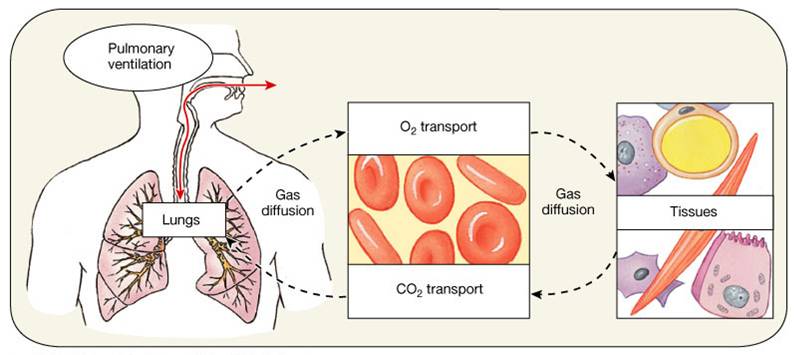
Respiration
Respiration consists of 4 distinct processes:
- Pulmonary Ventilation
- moving air into and out of the lungs.
- diaphragm and intercostals muscles promote ventilation
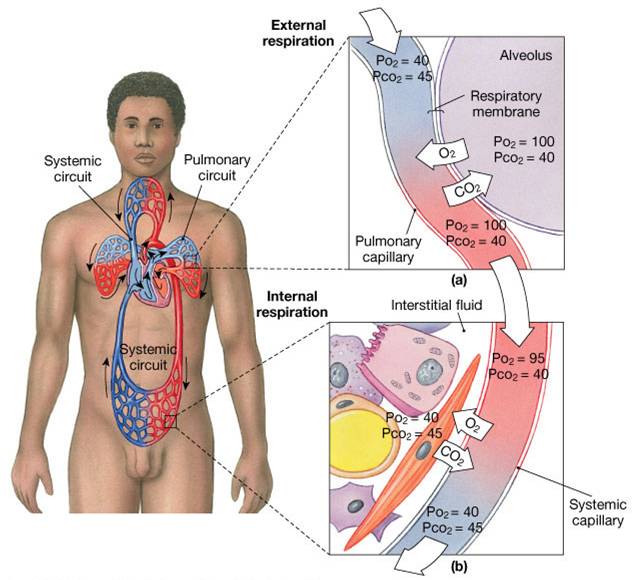
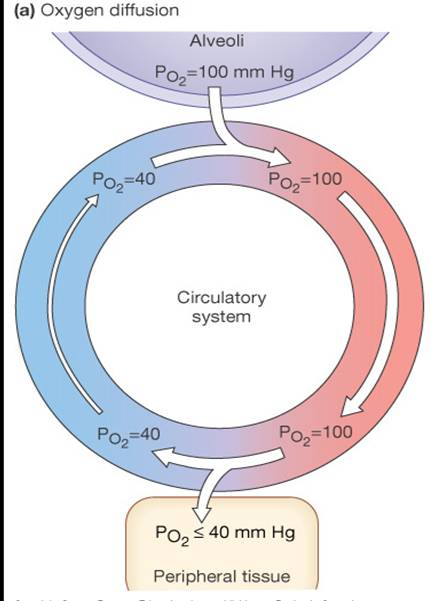
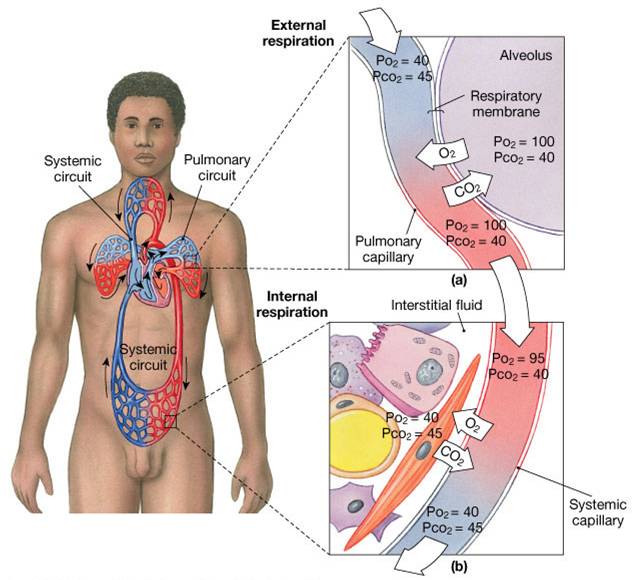
- External Respiration
- diffusion of gases between the alveoli and the blood of the pulmonary capillaries.
- Transport
- transport of oxygen and carbon dioxide between the lungs and tissues
- Internal Respiration
- diffusion of gases between the blood of the systemic capillaries and cells.
Click here to view an animation that summarizes internal and external respiration.
The animation is followed by practice questions.
1. Pulmonary Ventilation
Click here for an animation that summarizes the information that follows on pulmonary ventilation.
- The physical movement of air into and out of the lungs
- A mechanical process that depends on volume changes in the thoracic cavity
- Volume changes lead to pressure changes, which lead to the flow of gases in and out of the thoracic cavity to equalize pressure
- Includes inspiration and expiration
- *Gases move from areas of high pressure to areas of low pressure
|
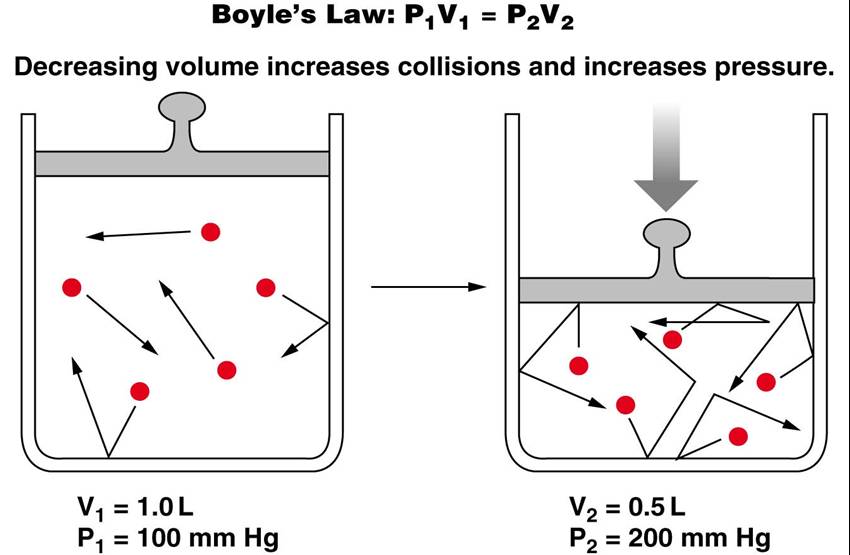
Boyle’s Law
Boyle's Law states that the relationship between the pressure and volume of gases is inversely proportional for a gas held at a constant temperature
P1V1 = P2V2
P = pressure of a gas in mm Hg
V = volume of a gas in cubic millimeters
That is :
- as pressure decreases, volume increases
- as volume decreases, pressure increases
|
 |
Thoracic Volume Changes
- At rest the diaphragm is relaxed
- As the diaphragm contracts, thoracic volume increases
- As the diaphragm relaxes, thoracic volume decreases
Pressure Relationships in the Thoracic Cavity
- Respiratory pressure is always described relative to atmospheric pressure
- Atmospheric pressure (ATM) - pressure exerted by all of the gases in the air we breathe (760 mm Hg at sea level)
Negative respiratory pressure is less than ATM
Positive respiratory pressure is greater than ATM
- Intrapulmonary pressure
- pressure within the alveoli ~760mmHg (when even with ATM )
- ntrapulmonary pressure always eventually equalizes itself with atmospheric pressure
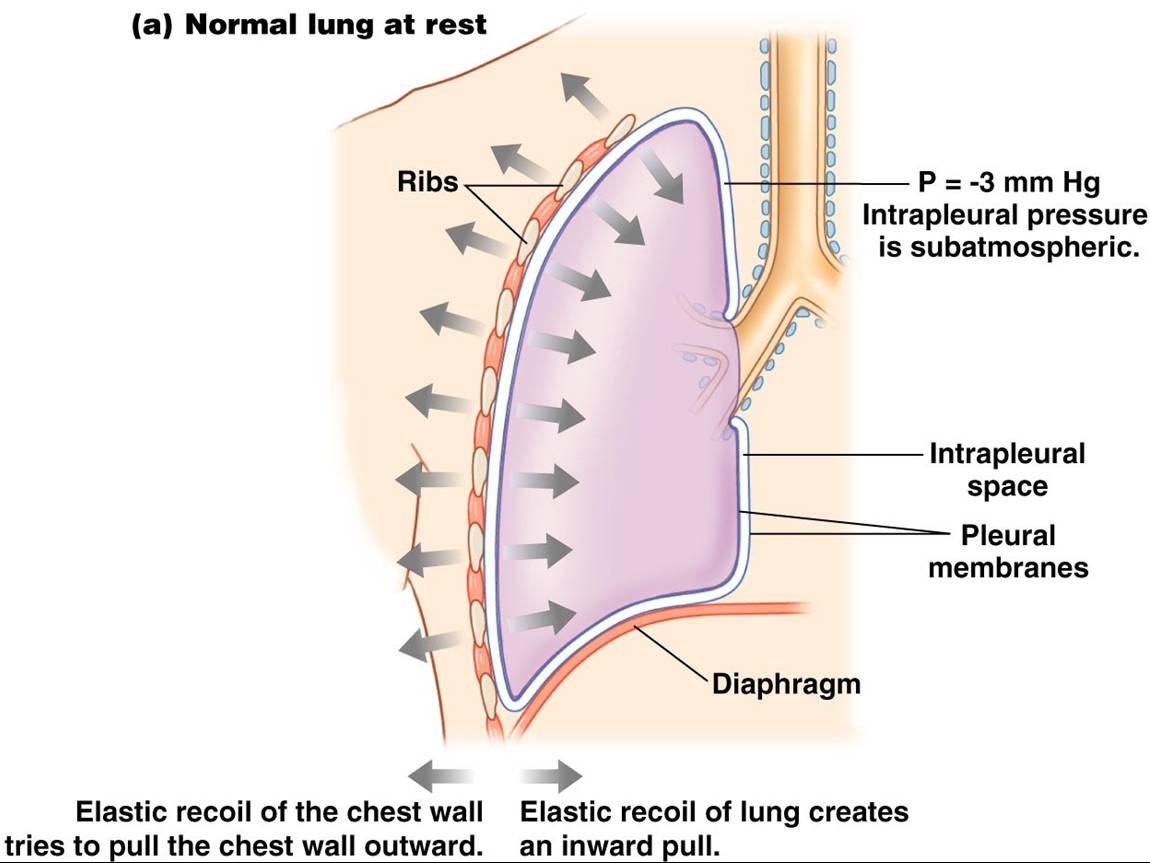
- Intrapleural pressure
- pressure within the pleural cavity which adheres lungs to thoracic cavity ~ 756mmHg
- intrapleural pressure is always less than intrapulmonary pressure and atmospheric pressure
- Intrapulmonary pressure and intrapleural pressure fluctuate with the phases of breathing
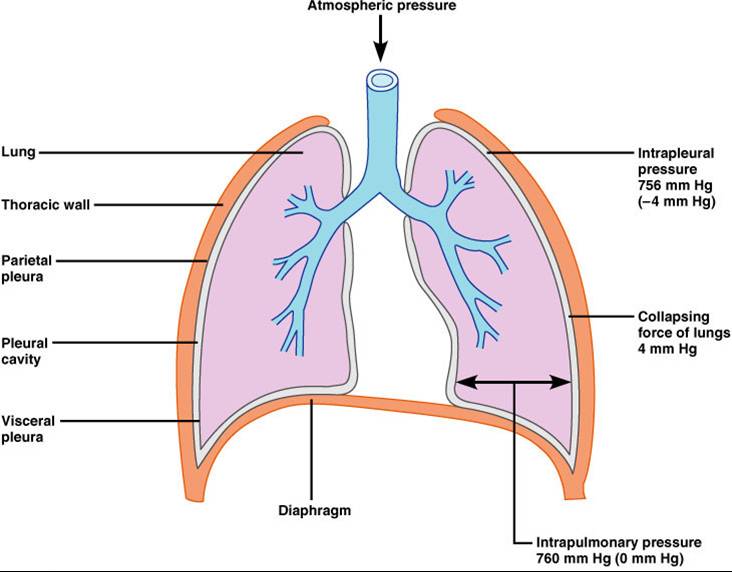
2 forces hold the thoracic wall and lungs in close apposition – stretching the lungs to fill the large thoracic cavity
- Intrapleural fluid cohesiveness – polarity of water attracts wet surfaces
- Transmural pressure gradient – pATM (760mmHg) is greater than intrapleural pressure (756mmHg) so lungs expand
 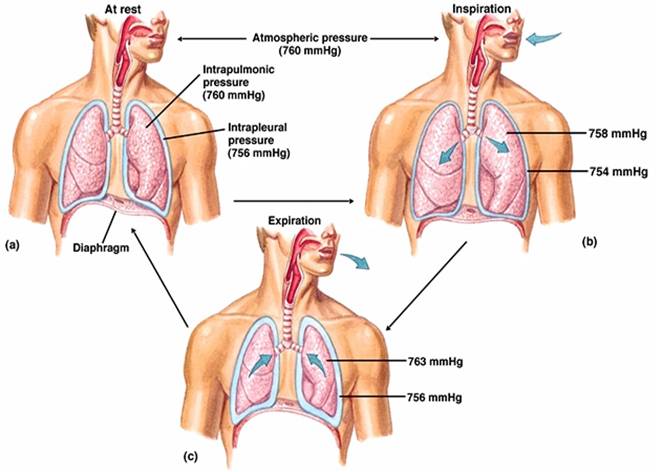
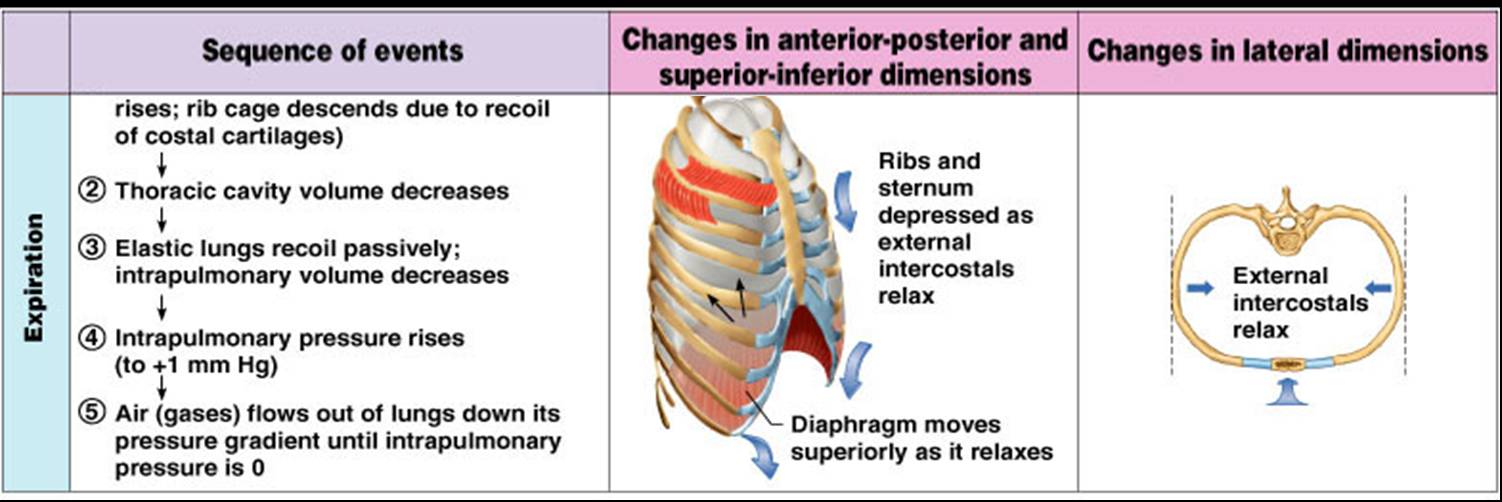
Inspiration
- The diaphragm and external intercostal muscles (inspiratory muscles) contract and the rib cage rises, stretching the lungs and increasing intrapulmonary volume.
- Intrapulmonary pressure drops below atmospheric pressure (1 mm Hg) drawing air flow into the lungs, down its pressure gradient, until intrapleural pressure = atmospheric pressure
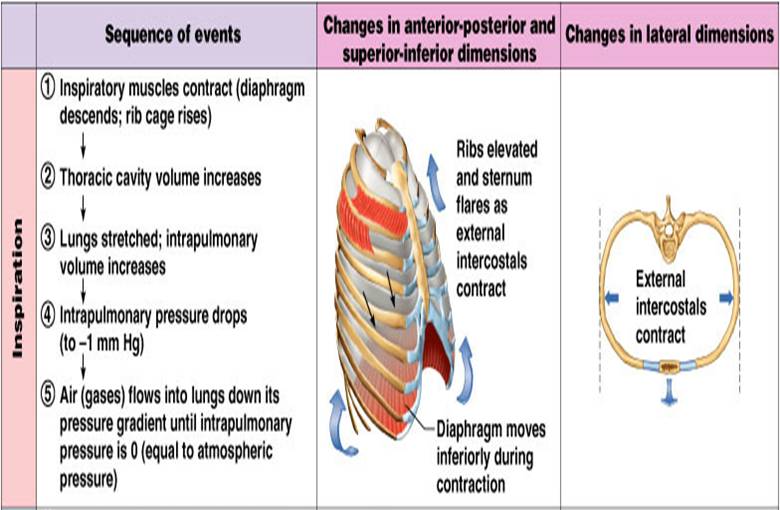
Expiration
- Inspiratory muscles relax and the rib cage descends due to gravity, elasticity.
- Thoracic cavity volume decreases, elastic lungs recoil passively and intrapulmonary volume decreases.
- Intrapulmonary pressure rises above atmospheric pressure (+1 mm Hg), gases flow out of the lungs down the pressure gradient until intrapulmonary pressure is 0
Respiratory Cycle
- Single cycle of inhalation and exhalation
- Amount of air moved in one cycle = tidal volume

Physical Factors Influencing Ventilation
Friction
- Is the major nonelastic source of resistance to airflow
- The relationship between flow (F), pressure (P), and resistance (R) is
Flow = ΔP /R
Compliance
- Is the ability to stretch, the ease with which lungs can be expanded due to change in transpulmonary pressure
- Is determined by 2 main factors:
- Distensibility of the lung tissue and surrounding thoracic cage
- Surface tension of the alveol
- High compliance - stretches easily
- Low compliance - Requires more force
- Restrictive lung diseases - fibrotic lung diseases and inadequate surfactant production
Elastic Recoil
- Is how readily the lungs rebound after being stretched
- Elasticity of connective tissue causes lungs to assume smallest possible size
- Surface tension of alveolar fluid draws alveoli to their smallest possible siz
Elastance
- Is returning to its resting volume when stretching force is released
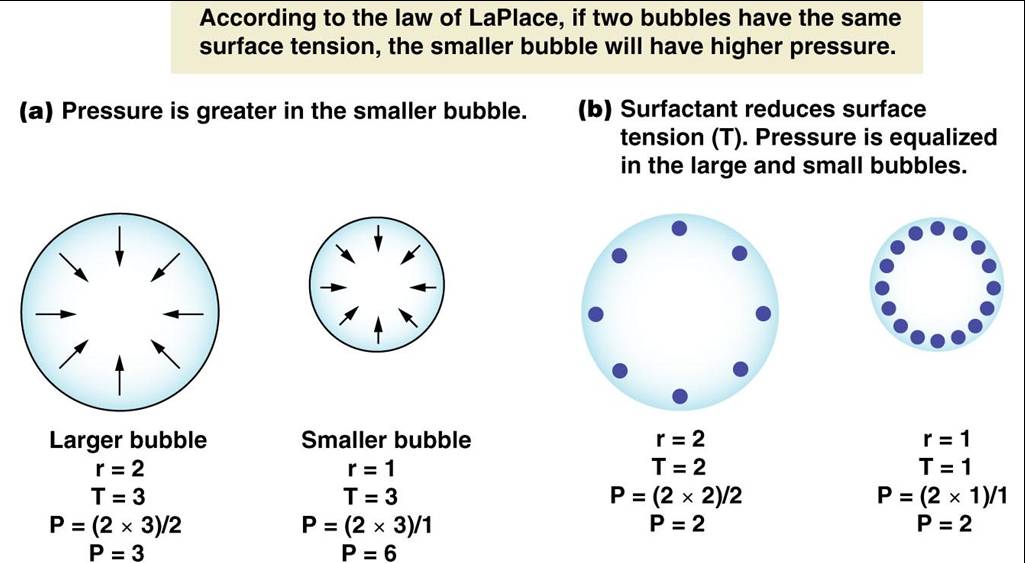
Surface Tension
- Is the attraction of liquid molecules to one another at a liquid-gas interface, the thin fluid layer between alveolar cells and the air
- This liquid coating the alveolar surface is always acting to reduce the alveoli to the smallest possible size
- Surfactant, a detergent-like complex secreted by Type II alveolar cells, reduces surface tension and helps keep the alveoli from collapsing
|
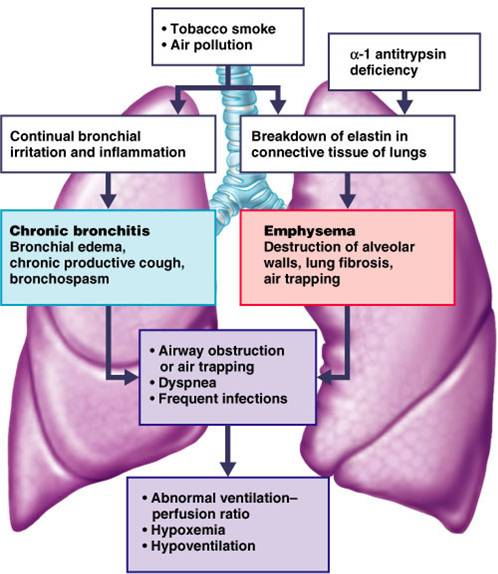
Airway Resistance
- Gas flow is inversely proportional to resistance with the greatest resistance being in the medium-sized bronchi,
- Severely constricted or obstructed bronchioles: COPD
|
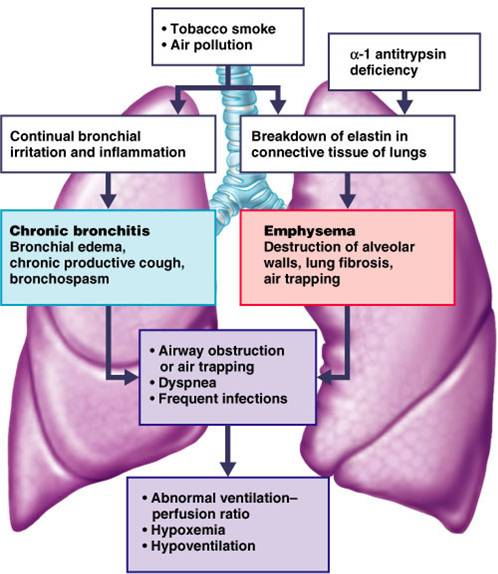 |
Diseases of the Lungs
- Emphysema--destruction of alveoli reduces surface area for gas exchange
- Fibrotic lung disease--thickened alveolar membrane slows gas exchange, loss of lung compliance
- Pulmonary edema--fluid in interstitial space increases diffusion distance
- Asthma--increased airway restriction decreases airway ventilation
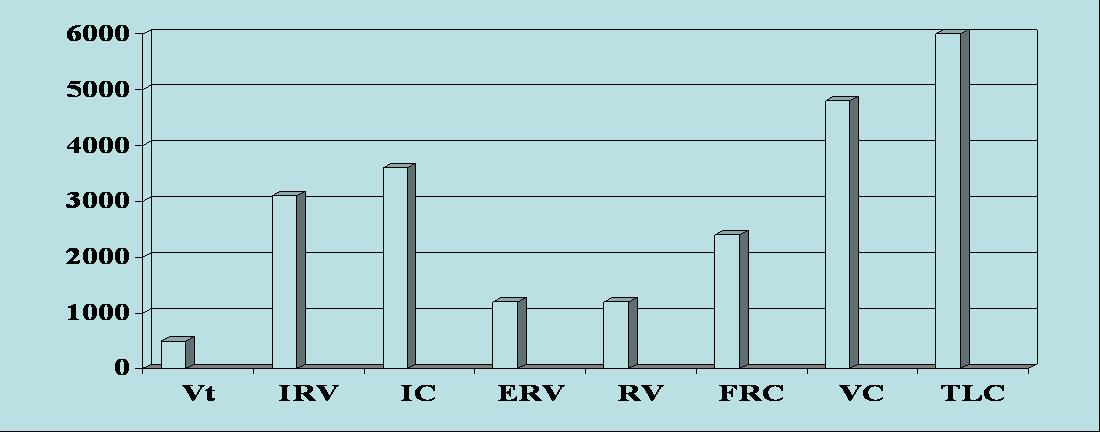
Lung Capacities and Volumes
- Tidal volume (TV) – air that moves into and out of the lungs with each breath (approximately 500 ml)
- Inspiratory reserve volume (IRV) – air that can be inspired forcibly beyond the tidal volume (2100–3200 ml)
- Expiratory reserve volume (ERV) – air that can be evacuated from the lungs after a tidal expiration (1000–1200 ml)
- Residual volume (RV) – air left in the lungs after strenuous expiration (1200 ml)
- Inspiratory capacity (IC) – total amount of air that can be inspired after a tidal expiration (IRV + TV)
- Functional residual capacity (FRC) – amount of air remaining in the lungs after a tidal expiration
(RV + ERV)
- Vital capacity (VC) – the total amount of exchangeable air (TV + IRV + ERV)
- Total lung capacity (TLC) – sum of all lung volumes (approximately 6000 ml in males)
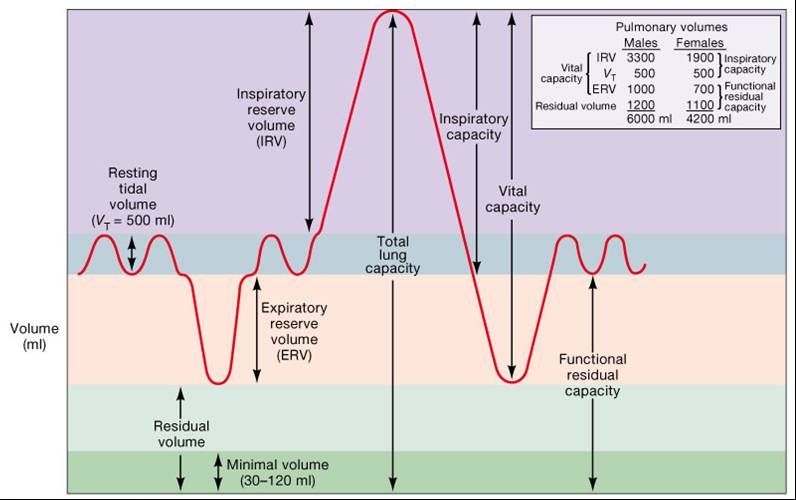
Dead Space
- Anatomical dead space – volume of the conducting respiratory passages (150 ml)
- Alveolar dead space – alveoli that cease to act in gas exchange due to collapse or obstruction
- Total dead space – sum of alveolar and anatomical dead spaces
|
|
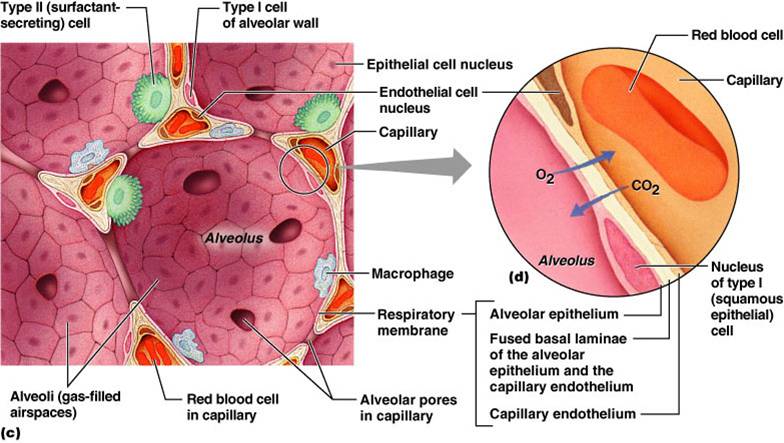
External Respiration: Pulmonary Gas Exchange
- Factors influencing the movement of oxygen and carbon dioxide across the respiratory membrane
- Partial pressure gradients and gas solubilities
- Matching of alveolar ventilation and pulmonary blood perfusion
- Structural characteristics of the respiratory membrane
Click here for an animation that reviews the structure of the alveoli and describes external respiration. |
 |
|
Gas Properties
Dalton’s Law
Total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture
- The partial pressure of each gas is directly proportional to its percentage in the mixture
- The partial pressure of oxygen (PO2)
- Air is 20.93% oxygen
- Total pressure of air = 760 mmHg
- PO2 = 0.2093 x 760 = 159 mmHg
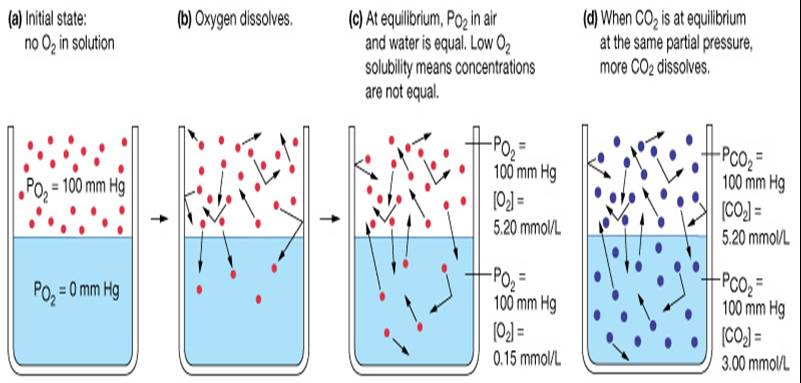
Henry's Law
When a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure
- The amount of gas that will dissolve in a liquid also depends upon its solubility
- Various gases in air have different solubilities:
- Carbon dioxide is the most soluble
- Oxygen is 1/20th as soluble as carbon dioxide
- Nitrogen is practically insoluble in plasma
Diffusion of Gases
Gases diffuse from high to low partial pressure
--Between lung and blood
--Between blood and tissue
- Fick’s law of diffusion:
V gas = A x D x (P1-P2)
T
- V gas = rate of diffusion
- A = tissue area
- T = tissue thickness
- D = diffusion coefficient of gas
- P1-P2 = difference in partial pressure
Respiratory Membranes
2. Type II (Septal) Cells
- Are few in number and are found between type I alveolar cells
- Are rounded or cuboidal epithelial cells whose free surfaces contain microvilli
- These cells secrete alveolar fluid keeps the surface between the cells and the air moist
- Part of the alveolar fluid is surfactant a mixture of phospholipids and lipoproteins that lowers the surface tension of the alveolar fluid, which reduces the tendency of the alveoli to collapse
3. Alveolar Macrophages (Dust Cells)
- Are associated with the alveolar wall
- Are wandering phagocytes that remove fine dust particles and other debris in the alveolar spaces. engulf foreign particle
Click here for an animation that reviews the structure of respiratory membranes. Review the first half of the animation.
Composition of Alveolar Gas
- The atmosphere is mostly nitrogen ~79% & oxygen ~21%, only 0.03% is CO2
- Alveoli contain more CO2 and water vapor
- These differences result from:
- Gas exchanges in the lungs – oxygen diffuses from the alveoli and carbon dioxide diffuses into the alveoli
- Humidification of air by conducting passages
- The mixing of alveolar gas that occurs with each breath
- Based on Dalton’s law, partial pressure of alveolar oxygen is 100mmHG and partial pressure of alveolar CO2 is 40mmHg
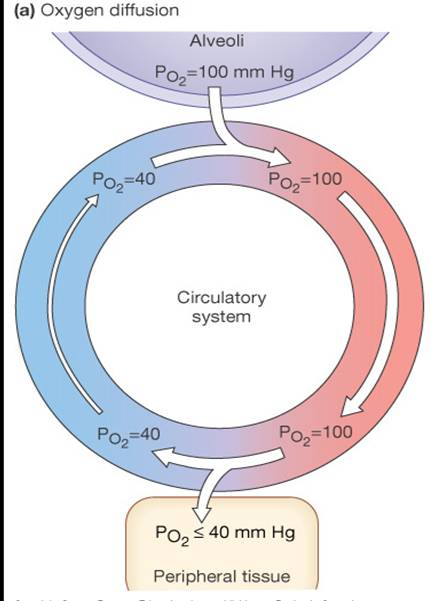
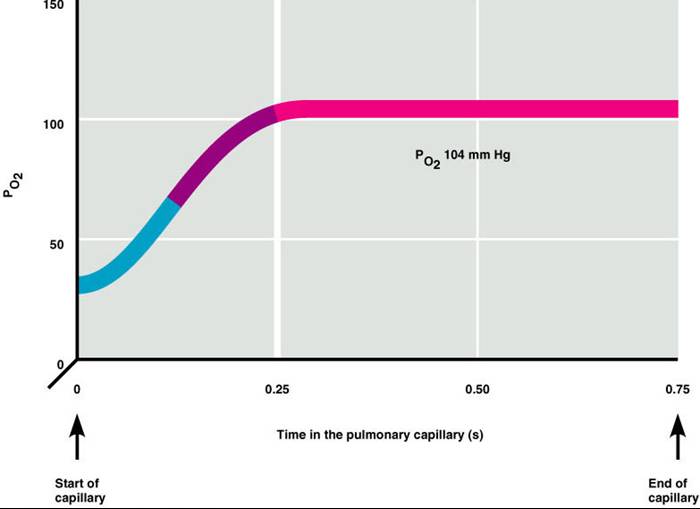
Partial Pressure Gradients
- The partial pressure of oxygen (PO2) of venous blood is 40 mm Hg
- The PO2 in the alveoli is ~100 mm Hg
- Steep gradient allows PO2 gradients to rapidly reach equilibrium (0.25sec)
- Blood can move quickly through the pulmonary capillary and still be adequately oxygenated
|
|
 |
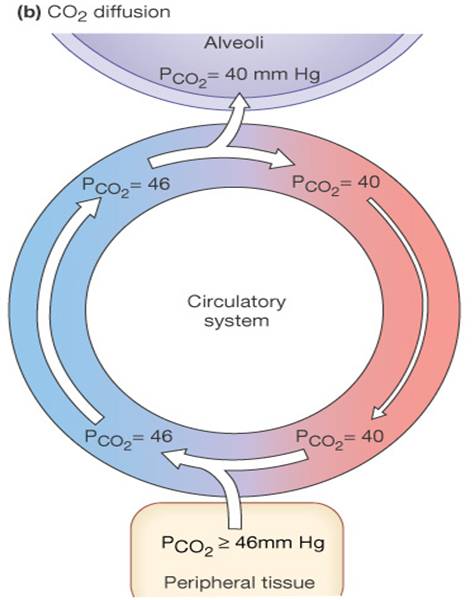
- Although carbon dioxide has a lower partial pressure gradient 40 -> 46:
- It is 20 times more soluble in plasma than oxygen
- It diffuses in equal amounts with oxygen
|
Internal Respiration
- The factors promoting gas exchange between systemic capillaries and tissue cells are the same as those acting in the lungs
- The partial pressures and diffusion gradients are reversed
- PO2 in tissue is always lower than in systemic arterial blood
- PO2 of venous blood draining tissues is 40 mm Hg and PCO2 is 45 mm Hg
Click here for an animation that reviews how internal respiration occurs. |
 |
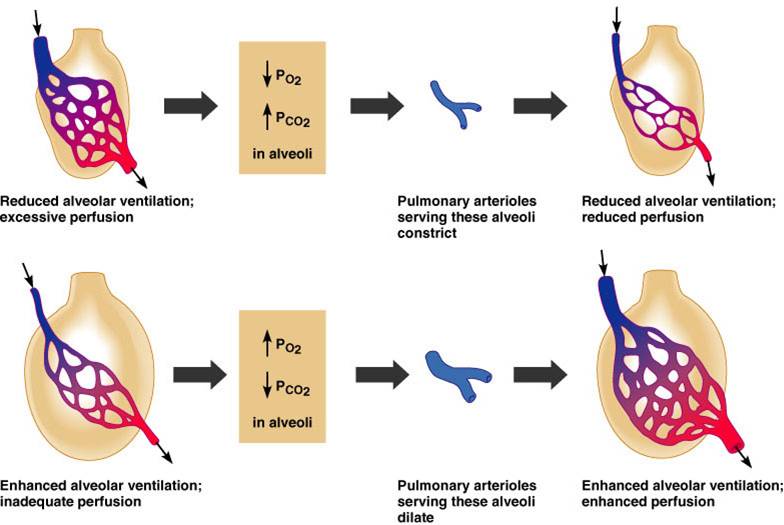
Ventilation-Perfusion Coupling
- Ventilation – the amount of gas reaching the alveoli
- Perfusion – the blood flow reaching the alveoli
- Ventilation and perfusion must be tightly regulated for efficient gas exchange
- Changes in PCO2 in the alveoli cause changes in the diameters of the pulmonary arterioles
- Alveolar CO2 is high/O2 low: vasoconstriction
- Alveolar CO2 is low/O2 high: vasodilation
|
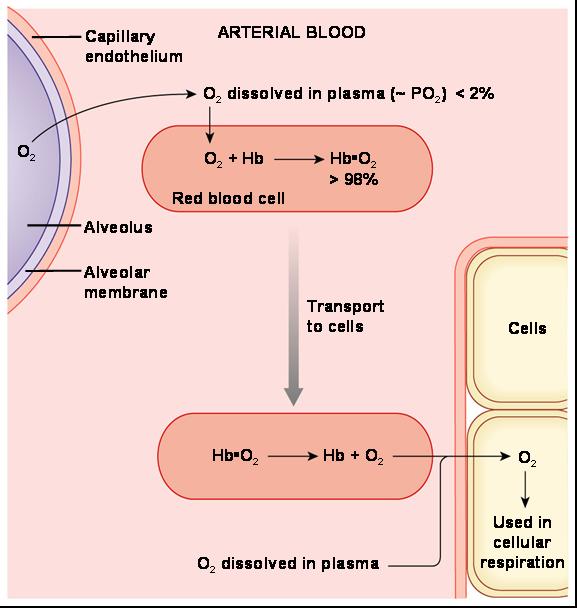
O2 Transport in the Blood
- Dissolved in plasma
- Bound to hemoglobin (Hb) for transport in the blood
- Oxyhemoglobin: O2 bound to Hb (HbO2)
- Deoxyhemoglobin: O2 not bound to (HHb)
- Carrying capacity
- 201 ml O2 /L blood in males
- 150 g Hb/L blood x 1.34 ml O2 / /g of Hb
- 174 ml O2 /L blood in females
- 130 g Hb/L blood x 1.34 mlO2/g of Hb
|
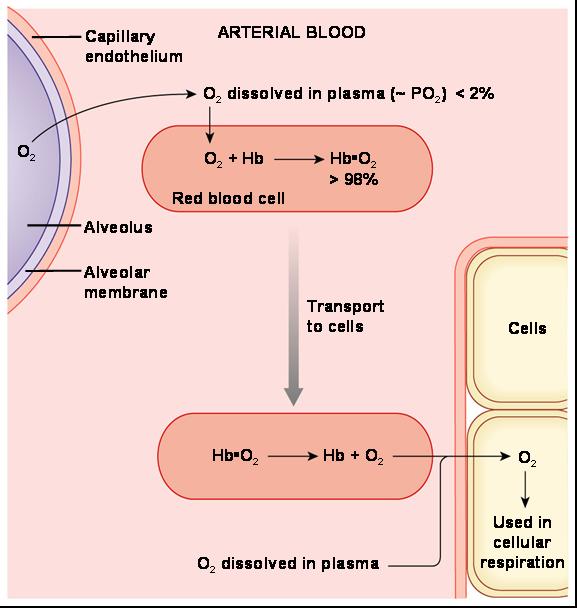 |
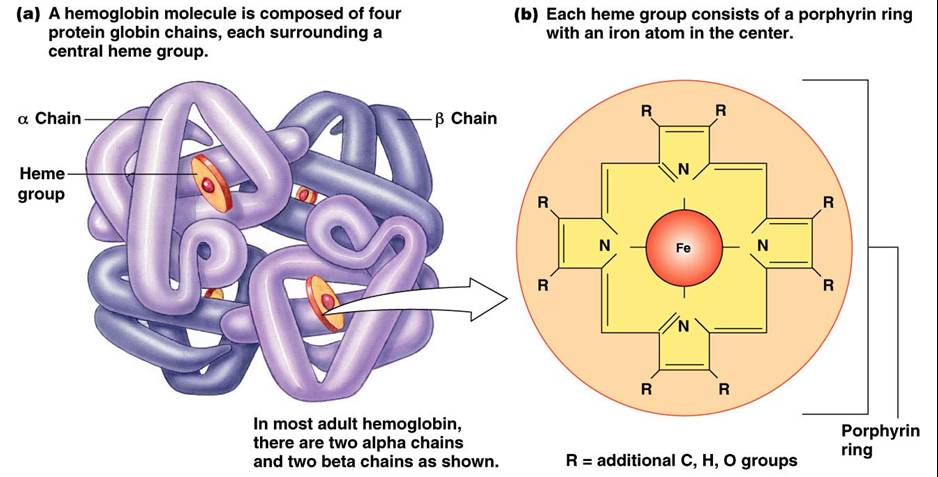
Hemoglobin (Hb)
- Saturated hemoglobin – when all four hemes of the molecule are bound to oxygen
- Partially saturated hemoglobin – when one to three hemes are bound to oxygen
- Rate that hemoglobin binds and releases oxygen is regulated by:
- PO2
- Temperature
- Blood pH
- PCO2
- [2,3 DPG] (an organic chemical)
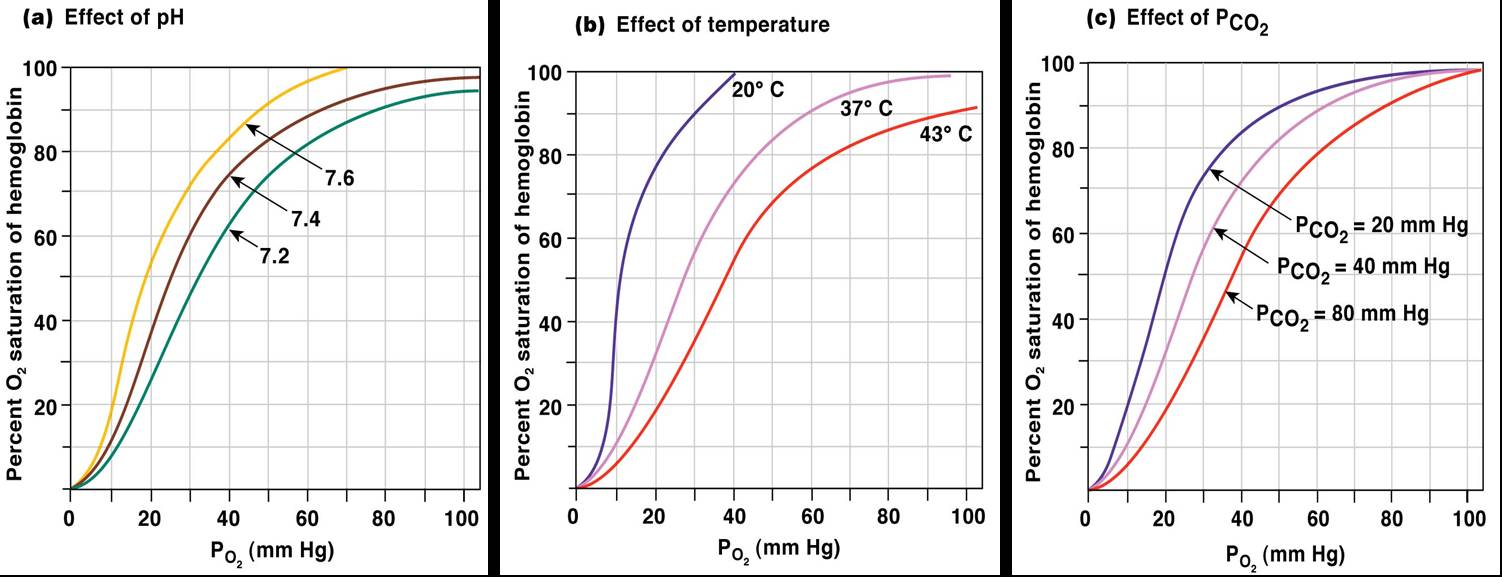
Hemoglobin Saturation Curve
Hemoglobin saturation plotted against PO2 produces a oxygen-hemoglobin dissociation curve:
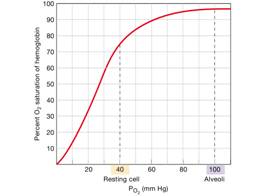
- At 100mmHg, hemoglobin is 98% saturated
- Saturation of hemoglobin is why hyperventilation has little effect on arterial O2 levels
- In fact, hemoglobin is almost completely saturated at a PO2 of 70 mm Hg
- Further increases in PO2 produce only small increases in oxygen binding
- Oxygen loading and delivery to tissue is still adequate when PO2 is below normal levels
Influence of PO2 on Hemoglobin Saturation
- 98% saturated arterial blood contains 20 ml oxygen per 100 ml blood (20 vol %)
- Only 20–25% of bound oxygen is unloaded during one systemic circulation
- As arterial blood flows through capillaries, 5 ml oxygen/dl are released
- If oxygen levels in tissues drop:
- More oxygen dissociates from hemoglobin and is used by cells
- Respiratory rate or cardiac output need not increase
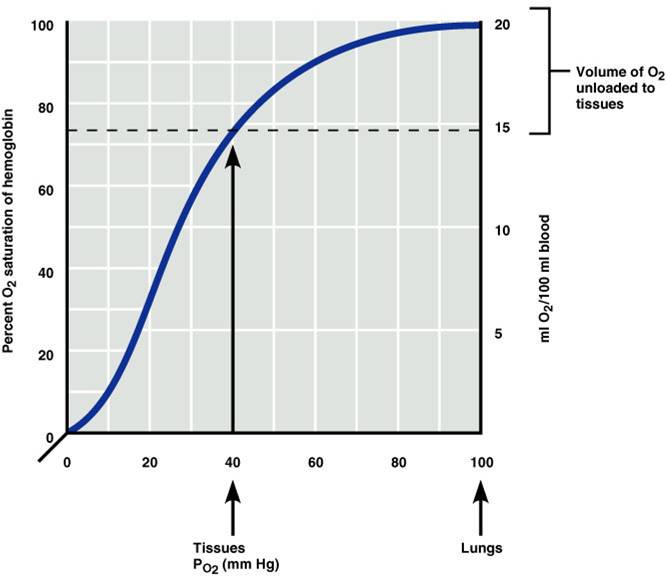
Factors Influencing Hb Saturation
- Temperature
- H+ ion concentration
- PCO2
- BPG
- Increases of these factors decrease hemoglobin’s affinity for oxygen and enhance oxygen unloading from the blood
- H+ and CO2 modify the structure of Hb - Bohr effect
- DPG produced by RBC metabolism when environmental O2 levels are low
- These parameters are all high in systemic (tissue) capillaries where oxygen unloading is the goal
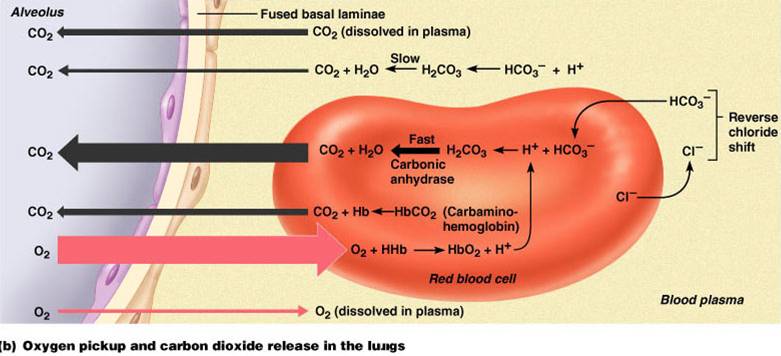
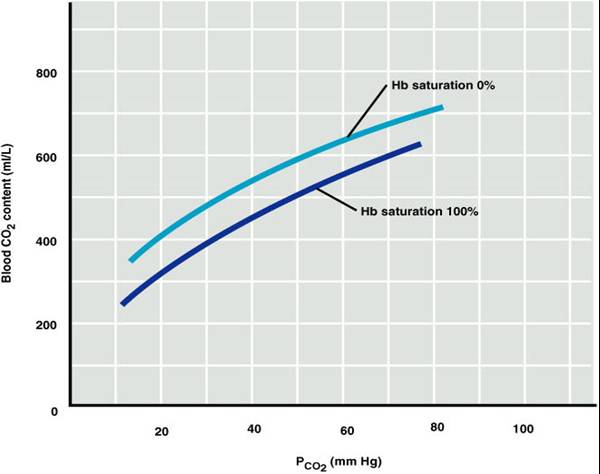
Carbon Dioxide Transport
Carbon dioxide is transported in the blood in three forms
- Dissolved in plasma – 7 to 10%
- Chemically bound to hemoglobin – 20% is carried in RBCs as carbaminohemoglobin
- Bicarbonate ion in plasma – 70% is transported as bicarbonate (HCO3–)
Transport and Exchange of CO2
- Carbon dioxide diffuses into RBCs and combines with water to form carbonic acid (H2CO3), which quickly dissociates into hydrogen ions and bicarbonate ions
- In RBCs, carbonic anhydrase reversibly catalyzes the conversion of CO2 and water to carbonic acid
- carbonic acid–bicarbonate buffer system resists blood pH changes
If [H+] in blood increases, excess H+ is removed by combining with HCO3–
If [H+] decrease, carbonic acid dissociates, releasing H+
Chloride Shift
At the tissues bicarbonate quickly diffuses from RBCs into the plasma
To counterbalance the out rush of negative bicarbonate ions from the RBCs, chloride ions (Cl–) move from the plasma into the erythrocytes. This is called chloride shift.

- At the lungs, these processes are reversed
- Bicarbonate ions move into the RBCs and bind with hydrogen ions to form carbonic acid
- Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water
- Carbon dioxide then diffuses from the blood into the alveoli
*Haldane Effect
- Removing O2 from Hb increases the ability of Hb to pick up CO2 and CO2 generated H+ is called the Haldane effect.
- The Haldane and Bohr effect work in synchrony to facilitate O2 liberation and uptake of CO2 and H+
- At the tissues, as more CO2 enters the blood:
- More oxygen dissociates from Hb (Bohr effect)
- Unloading O2 allows more CO2 to combine with Hb (Haldane effect), and more bicarbonate ions are formed
- This situation is reversed in pulmonary circulation
|
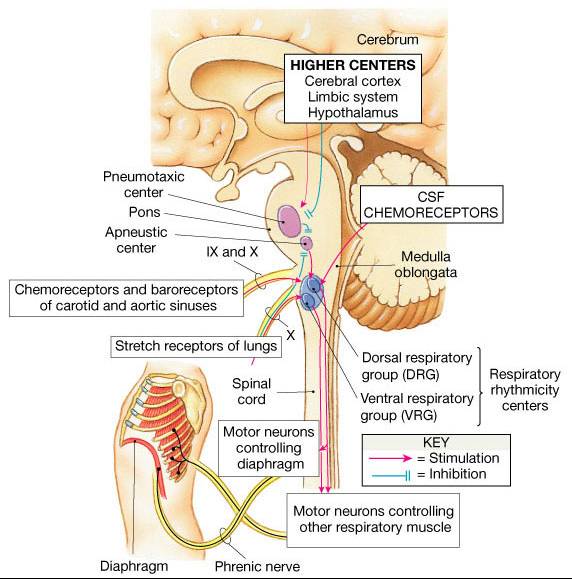
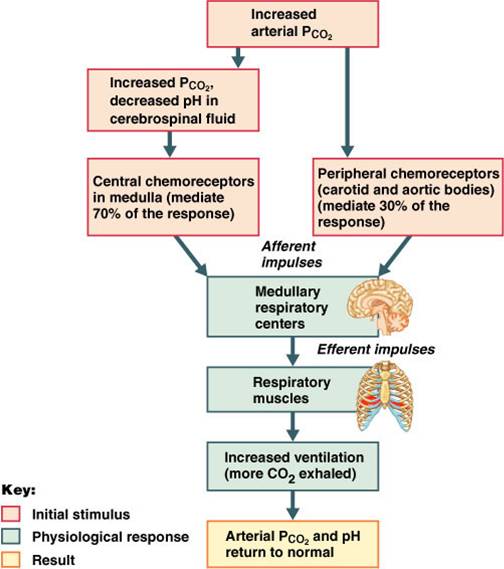
Control of Respiration
Clusters of specific neurons called respiratory centers control breathing. The centers located in the medulla oblongata set the rate and rhythm of normal breathing. The centers in the pons regulate the rate and depth of breathing.
Medullary Respiratory Centers
- Dorsal respiratory group (DRG), or inspiratory center:
- stimulates inhalations
- Inspiratory neurons
- Thought to set by basic rhythm “pacemaking” (now believed to be pre-Botzinger complex)
- Excites the inspiratory muscles and sets eupnea (12-15 breaths/minute)
- Cease firing during expiration
- Ventral respiratory group (VRG) or expiratory center
- Inspiratory & expiratory neurons
- Remains inactive during quite breathing
- Activity when demand is high
- Involved in forced inspiration and expiration
- Control via phrenic (to the diaphragm) and intercostal (to the external intercostal muscles) nerves
|
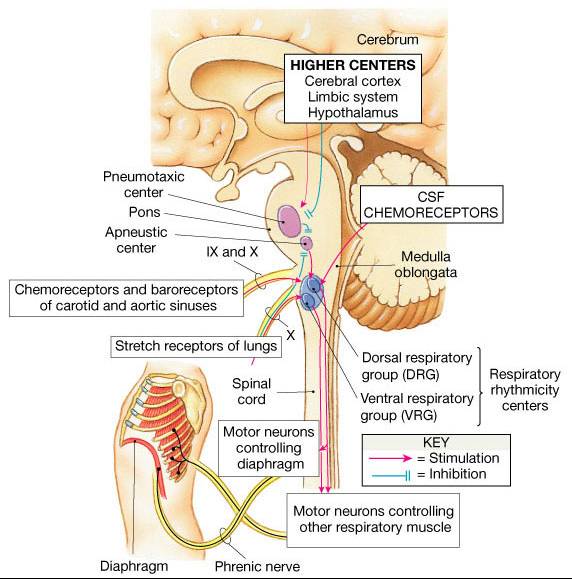 |
Pons Respiratory Centers
Influence and modify activity of the medullary centers to smooth out inspiration and expiration transitions
- Pneumotaxic center – this is the regulator; it coordinates the transition between inhalation and exhalation; it also prevents overinflation of the lungs by always sending inhibitory impulses to the inspiratory center (DRG)
- Apneustic center also coordinates the transition between inhalation and exhalation by fine-tuning the medullary respiratory centers; does this by sending stimulatory impulses to the inspiratory center (DRG) which result in a slower, deeper inhalation; this is necessary when you choose to hold your breath p
- Pneumotaxic centerdominates to allow expiration to occur normally
|
2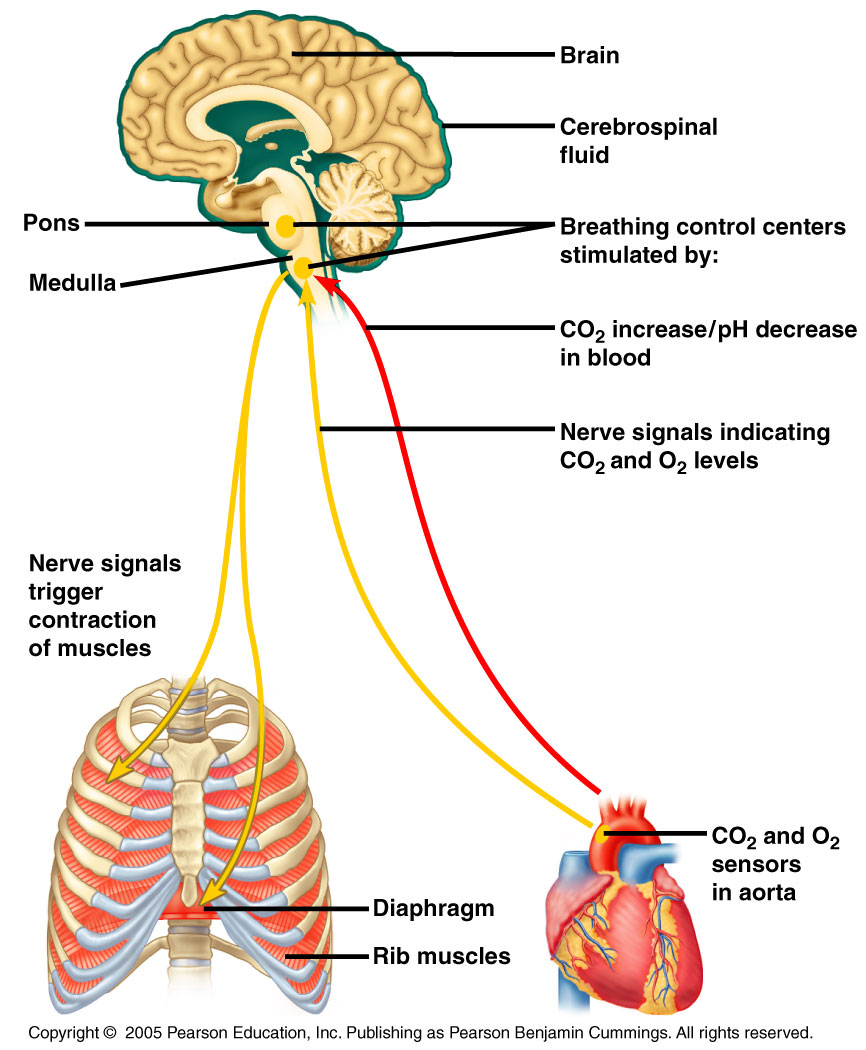 |
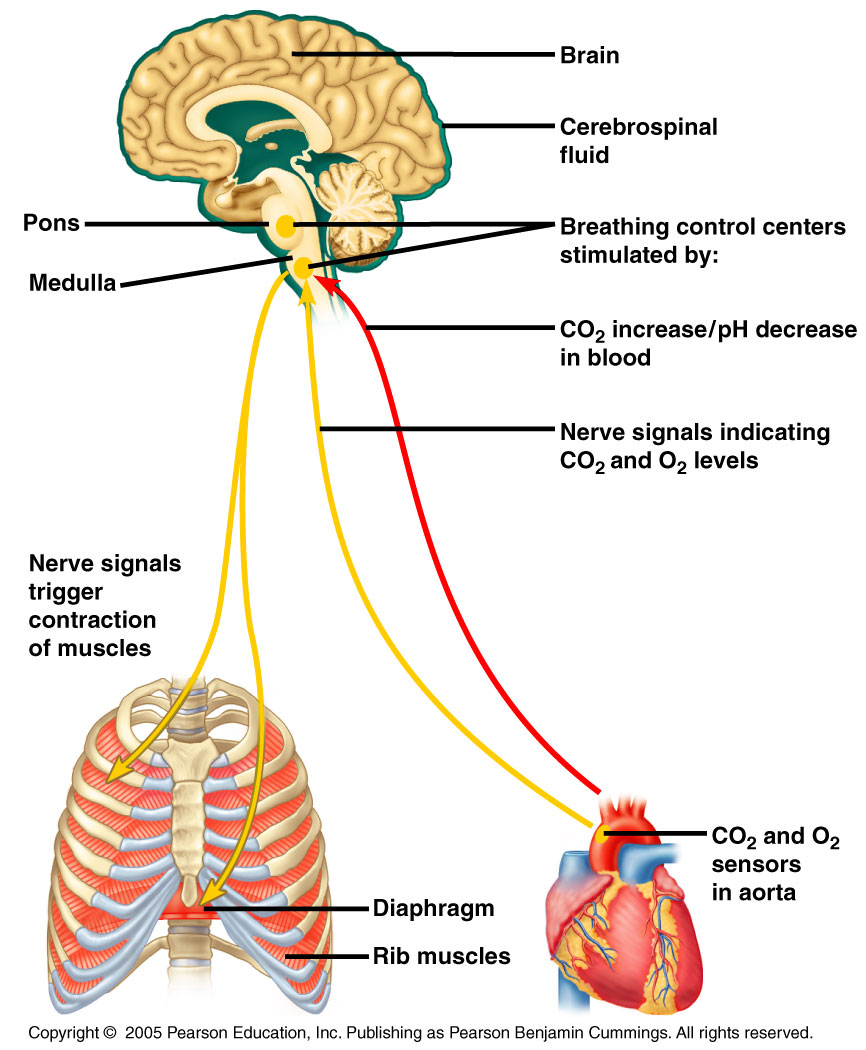
Depth and Rate of Breathing
- Inspiratory depth is determined by how actively the respiratory center stimulates the respiratory muscles
- Rate of respiration is determined by how long the inspiratory center is active
- Respiratory centers in the pons and medulla are sensitive to both excitatory and inhibitory stimuli
Input from chemoreceptors and stretch reflexes modify pacemaker activity
- Pulmonary irritant reflexes – irritants promote reflexive constriction of air passages
- Inflation reflex (Hering-Breuer) – stretch receptors in the lungs are stimulated by lung inflation
- Upon inflation, inhibitory signals are sent to the medullary inspiration center to end inhalation and allow expiration
- Hypothalamic controls act through the limbic system to modify rate and depth of respiration
- Example: breath holding that occurs in anger
- A rise in body temperature acts to increase respiratory rate
- Cortical controls are direct signals from the cerebral motor cortex that bypass medullary controls
- Examples: voluntary breath holding, taking a deep breath
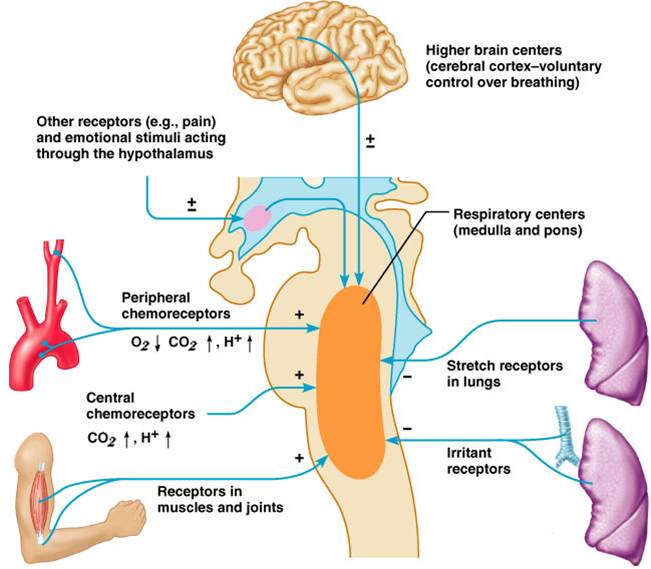
Depth and Rate of Breathing: PCO2
- Changing PCO2 levels are monitored by chemoreceptors of the brain stem
- Carbon dioxide in the blood diffuses into the cerebrospinal fluid where it is hydrated
- Resulting carbonic acid dissociates, releasing hydrogen ions
- PCO2 levels rise (hypercapnia) resulting in increased depth and rate of breathing
|
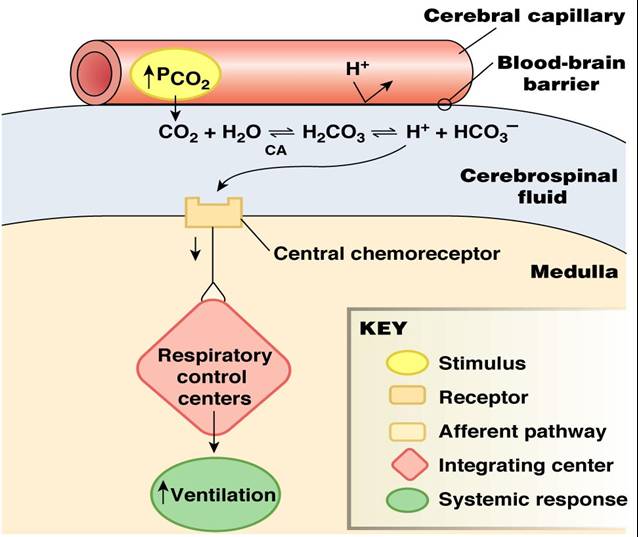
|
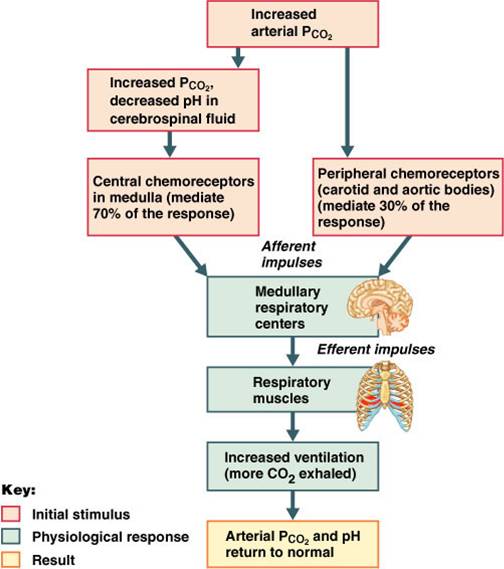 |
- Hyperventilation – increased depth and rate of breathing that:
- Quickly flushes carbon dioxide from the blood
- Occurs in response to hypercapnia
- Though a rise CO2 acts as the original stimulus, control of breathing at rest is regulated by the hydrogen ion concentration in the brain
- Hypoventilation – slow and shallow breathing due to abnormally low PCO2 levels
- Apnea (breathing cessation) may occur until PCO2 levels rise
- Arterial oxygen levels are monitored by the aortic and carotid bodies
- Substantial drops in arterial PO2 (to 60 mm Hg) are needed before oxygen levels become a major stimulus for increased ventilation
- If carbon dioxide is not removed (e.g., as in emphysema and chronic bronchitis), chemoreceptors become unresponsive to PCO2 chemical stimuli
- In such cases, PO2 levels become the principal respiratory stimulus (hypoxic drive)
Depth and Rate of Breathing: Arterial pH
- Changes in arterial pH can modify respiratory rate even if carbon dioxide and oxygen levels are normal
- Increased ventilation in response to falling pH is mediated by peripheral chemoreceptors
- Acidosis may reflect:
- Carbon dioxide retention
- Accumulation of lactic acid
- Excess fatty acids in patients with diabetes mellitus
- Respiratory system controls will attempt to raise the pH by increasing respiratory rate and depth
Top ...... Main Page |