Cardiovascular System (Blood Vessels)
|
Content
Physiology of Systemic Circulation
Blood Pressure
Resistance Factors
Blood Flow & Cross-Sectional Area
Vascular Tree
Arteries
Arterioles
Measuring Blood Pressure
Pulse Pressure
Veins
Capillaries
Atriovenous Anastomosis
Exchange of Fluid between Capillaries and Tissues
Fluid Movement
Lymphatic System
Intrinsic Regulation of Blood Flow (Autoregulation)
Extrinsic Regulation of Blood Flow
Blood Pressure Regulation
Regulation of Blood Pressure by ADH (Vasopressin)
Regulation of Blood Pressure by Atrial Natriuretic Peptide (ANP)
Cerebral Circulation
Perfusion = blood flow through tissues or organs |
Physiology of Systemic Circulation
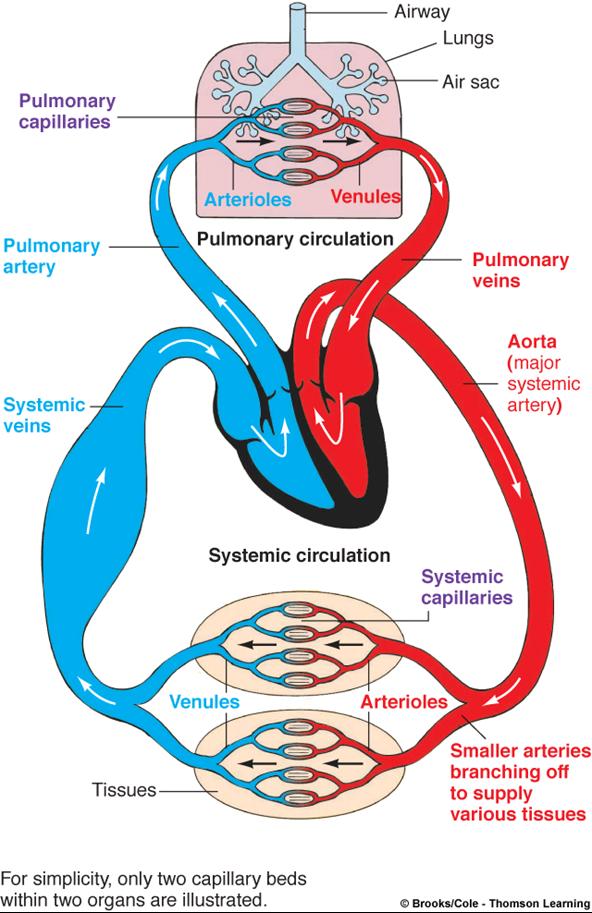
The systemic circulation is made up of the blood vessels that pump blood from the heart to the rest of the body. The pulmonary circulation is made up of the blood vessels that take deoxygenated blood from the right ventricle of the heart to the lung and then return oxygenated blood to the left atrium.
The physiology of the systemic circulation is determined by:
- Dynamics of blood flow
- Anatomy of circulatory system
- Regulatory mechanisms that control heart and blood vessels
Blood Volume
- Most in the veins (2/3rd)
- Smaller volumes in arteries and capillaries
Dynamics of Blood Circulation
Blood circulation involves interrelationships between
- Pressure
- Flow
- Resistance
- Control mechanisms that regulate blood pressure
- Blood flow through vessels
Volume of Blood Flow
The actual volume of blood flowing through a vessel, an organ, or the entire circulation in a given period is:
- Measured in ml per min.
- Equivalent to cardiac output (CO), considering the entire vascular system
- Relatively constant when at rest, varies widely through individual organs, according to immediate needs
Blood Pressure (BP)
- Force per unit area exerted on the wall of a blood vessel by its contained blood
- Expressed in millimeters of mercury (mm Hg)
- Measured in reference to systemic arterial BP in large arteries near the heart
- The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas
|
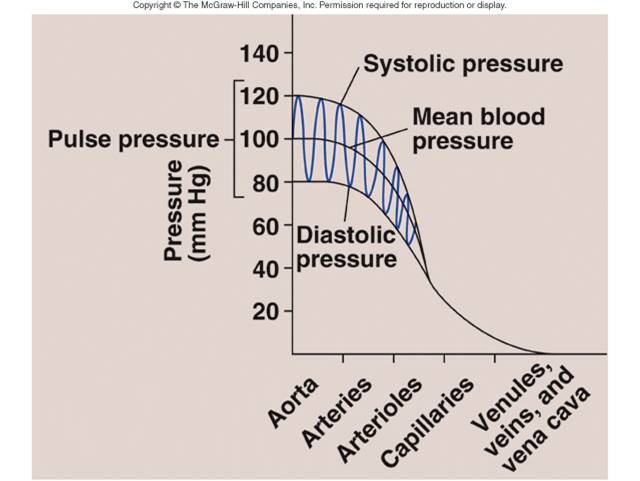
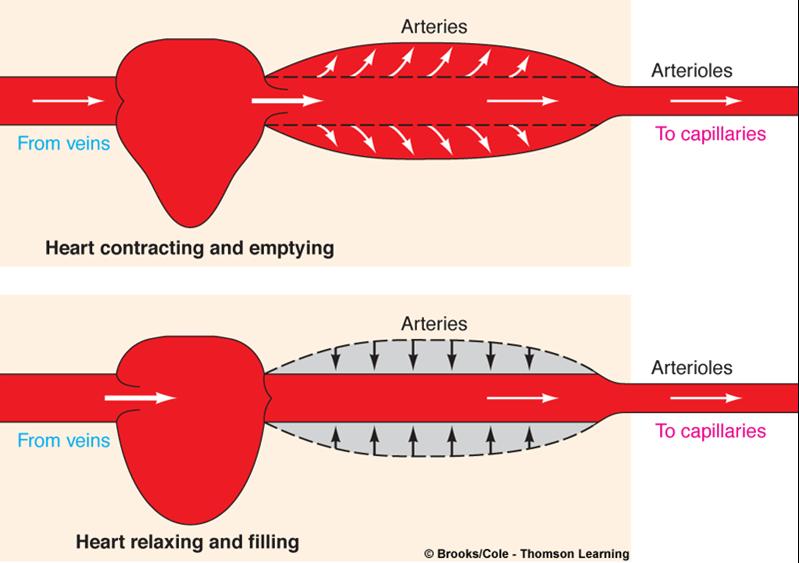
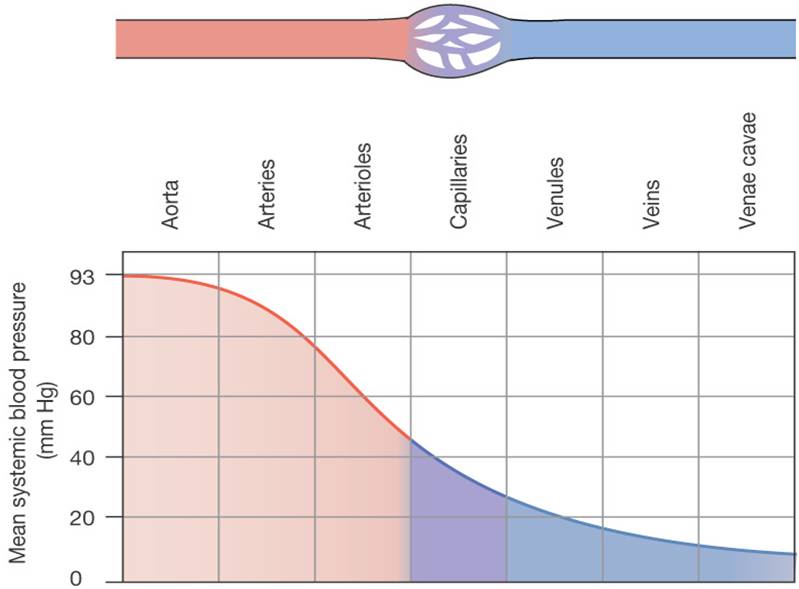
Blood Flow: Pressure Changes
- Flows down a pressure gradient
- Force of heart contraction
- Highest at the heart (driving P), decreases over distance
- Compliance (distensibility) of vessel
- Decreases 90% from aorta to vena cava
-
|
|
- Is directly proportional to pressure differences and inversely proportional to resistance.
Blood flow (F) is directly proportional to the difference in blood pressure (ΔP) between two points in the circulation, flows down a pressure gradient
Flow = ΔP /R
F = flow rate of blood through a vessel
ΔP = pressure gradient
R = resistance of blood vessels
R is more important than ΔP in influencing local blood pressure
|
|
Resistance Factors
- Constant factors
- Blood viscosity – thickness or “stickiness” of the blood; hematocrit, [plasma proteins]
- Blood vessel length – the longer the vessel, the greater the resistance encountered
- Dynamic Factors
- Blood vessel diameter
- Changes in vessel diameter significantly alter peripheral resistance
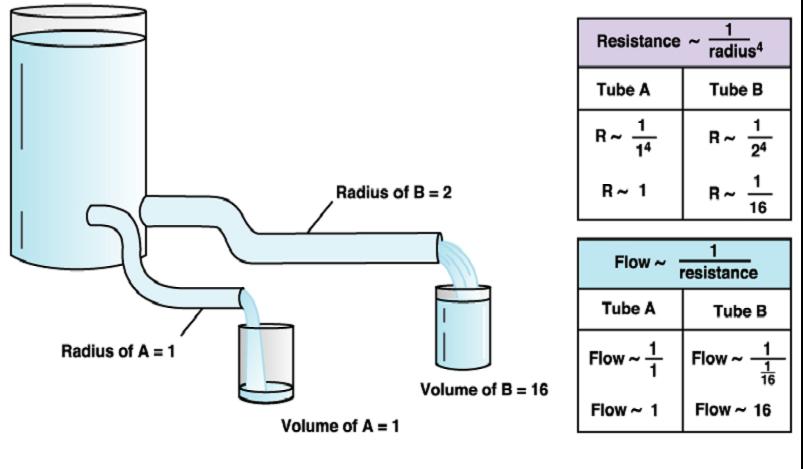
Resistance varies inversely with the fourth power of vessel radius (one-half the diameter).
- For example, if the radius is doubled, the resistance is 1/16 as much
- R = L n
r4
- L = length of the vessel
n = viscosity of blood
r = radius of the vessel
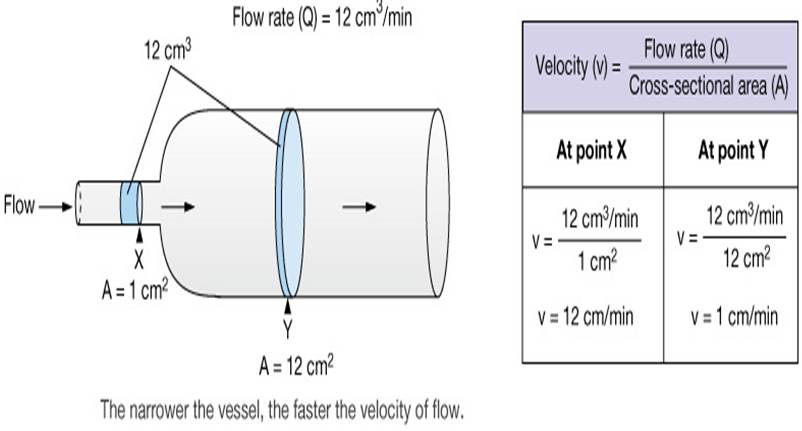
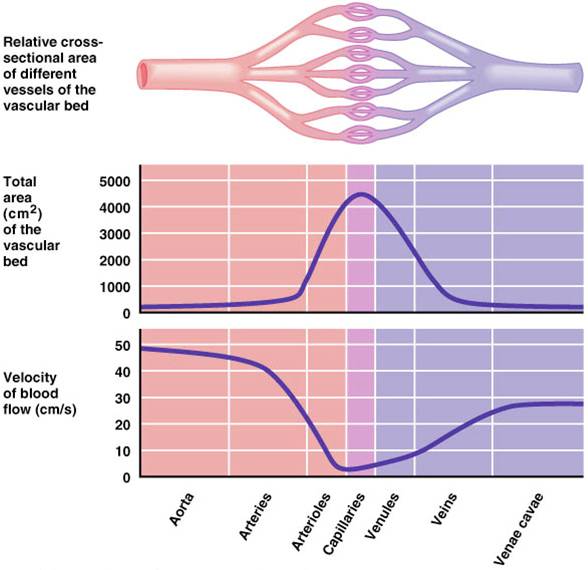
Blood Flow & Cross-Sectional Area
At the capillary bed:
- Vessel diameter decreases
- Number of vessels increase, increasing total cross-sectional area
- Velocity slows down so that capillaries can unload O2 and nutrients
Vascular Tree
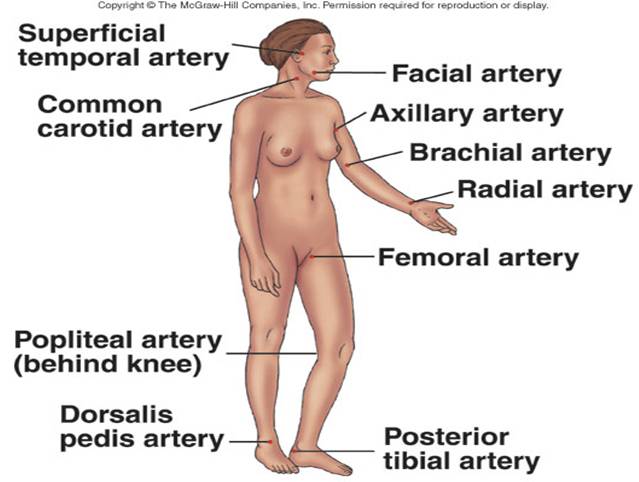
Is a closed system of vessels consisting of:
- Arteries
- Carry blood away from heart to tissues
- Arterioles
- Are smaller branches of arteries
- Capillaries
- Smaller branches of arterioles
- Smallest of vessels across which all exchanges are made with surrounding cells
- Venules
- Formed when capillaries rejoin
- Return blood to heart
- Veins
- Formed when venules merge
- Return blood to heart
 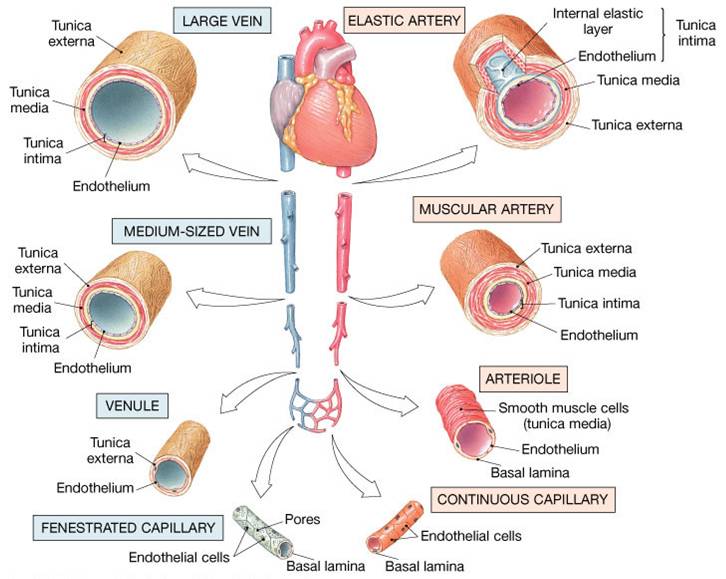
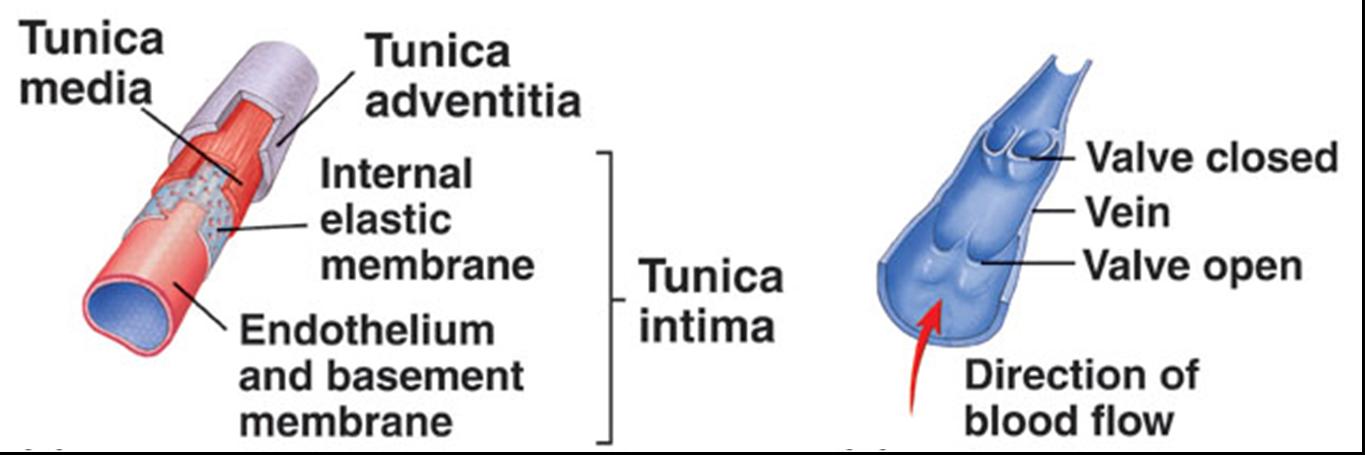
Arteries
There are 2 types of arteries:
1. Elastic or conducting arteries
- Largest in diameter
- Have high pressure fluctuations
- Provide pressure reservoir
- Elastic recoil propels blood after systole
2. Muscular or medium arteries
- Smooth muscle allows vessels to regulate blood supply by constricting or dilating
Arterioles
- Transport blood from small arteries to capillaries
- Control the amount of resistance
- Greatest drop in pressure occurs in arterioles which regulate blood flow through tissues
- No large fluctuations in capillaries and veins
Blood Pressure
- Is the force exerted by blood against a vessel wall
- Depends on
- Volume of blood forced into the vessel
- Compliance (distensibility/elasticity) of vessel walls
- Systolic Pressure
- Peak pressure exerted by ejected blood against vessel walls during cardiac systole (ventricular contraction)
- Averages 120 mm Hg
- Diastolic Pressure
- Minimum pressure in arteries when blood is draining off into vessels downstream, lowest level of arterial pressure during ventricular cycle
- Averages 80 mm Hg
- Blood pressure in elastic arteries near the heart is pulsatile (BP rises and falls)
- Mean Arterial Pressure (MAP)
- Is the average pressure that propels the blood to the tissues
- MAP = diastolic pressure + 1/3 pulse pressure
|
Critical closing pressure
Pressure at which a blood vessel collapses and blood flow stops
Laplace’s Law
Force acting on blood vessel wall is proportional to diameter of the vessel times blood pressure
|
|
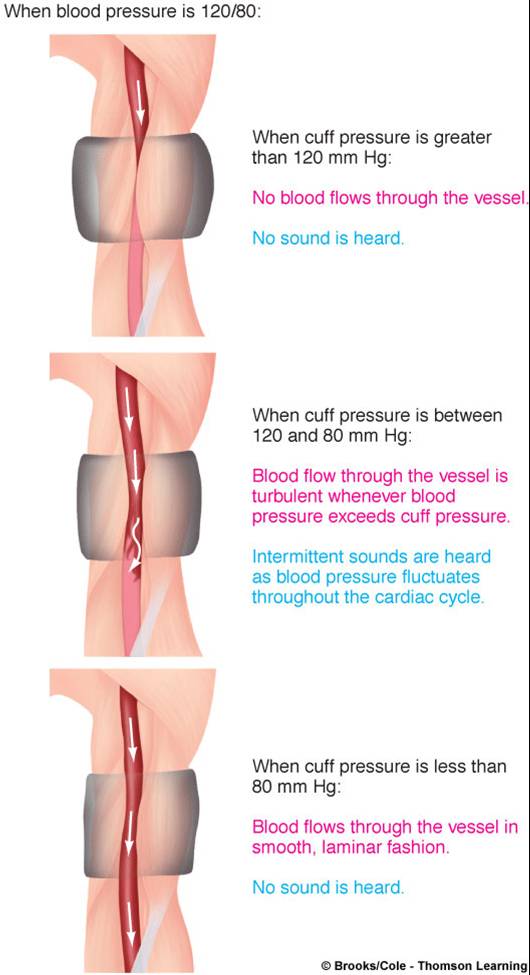
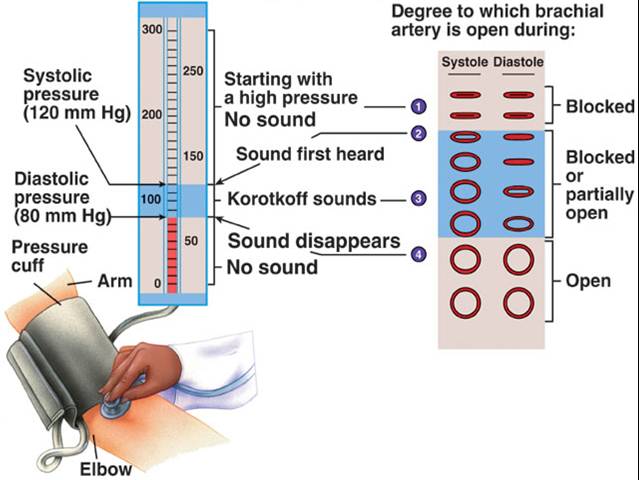
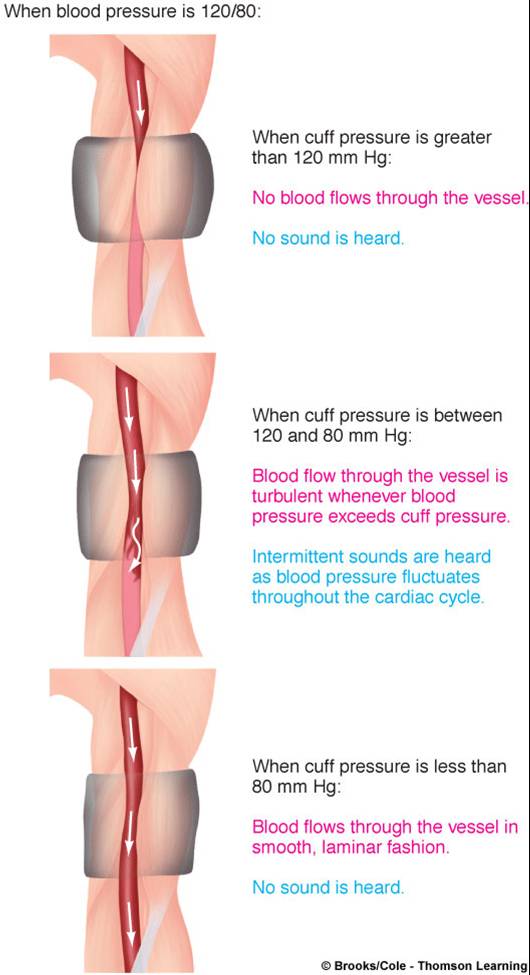
Measuring Blood Pressure
1. An inflatable cuff is placed around the arm so that the inflation of the cuff squeezes the brachial artery.
2. A stethoscope is placed over the artery distal to the cuff.
3. The cuff is inflated. (A tube connects the cuff to a pressure gauge that measures the pressure inside the cuff in millimeters of mercury (mm Hg).
Inflation is continued until cuff pressure is about 30 mm Hg above the pressure which is enough to cause the brachial artery to collapse, stop the flow of blood in the artery, and eliminate the sound of the pulse.
4. The air is slowly let out of the cuff. When the pressure in the cuff falls below systolic pressure, blood can again entery the artery.
At first, blood enters only at peak systolic pressure and the stethoscope picks up the sound of blood pulsing through the artery. The number at this point represents peak systolic pressure.
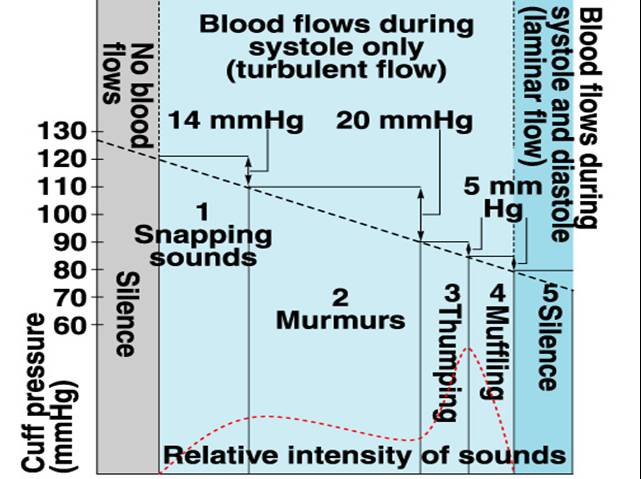
As the pressure falls further, the sound changes. When the cuff pressure falls below diastolic pressure, blood flow becomes continuous and the sound of the pulse becomes muffed or disappears completely. The number at this point indicates the diastolic pressure.
These sounds are called sounds of Korotkoff.
Blood pressure is recorded as the two numbers separated by a slash (e.g. 120/80. 120 is the systolic pressure and 80 is the diastolic pressure.
|
 |
Different phases in measurement of blood pressure are identified on the basis of the quality of the Korotkoff sounds.
Average arterial BP is 120/80 mm Hg.
Average pulmonary BP is 22/8 mm Hg.
Pulse Pressure
- Is the the difference between systolic and diastolic pressure
- Increases when stroke volume increases or vascular compliance decreases
- Can be used to take a pulse to determine heart rate and rhythmicity
- Effect of gravity on pulse pressure:
- In a standing position, hydrostatic pressure caused by gravity increases blood pressure below the heart and decreases pressure above the heart
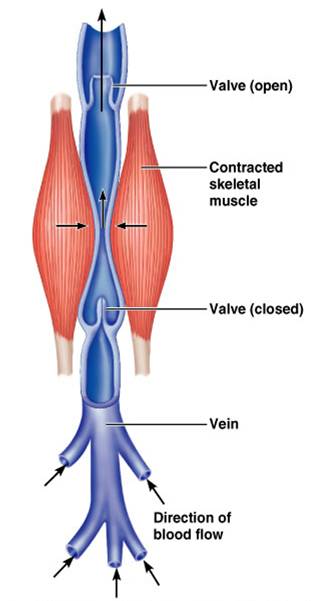
Veins
- Veins have much lower blood pressure and thinner walls than arteries
- To return blood to the heart, veins have special adaptations:
- Large-diameter lumens, which offer little resistance to flow
- Valves (resembling semilunar heart valves), which prevent backflow of blood
Venous Blood Pressure
- Is steady and changes little during the cardiac cycle
- The pressure gradient in the venous system is only about 20 mm Hg
- Veins have thinner walls, thus higher compliance.
- Vascular compliance
- Tendency for blood vessel volume to increase as blood pressure increases
- More easily the vessel wall stretches, the greater its compliance
- Venous system has a large compliance and acts as a blood reservoir
- Are cpacitance vessels - 2/3 of blood volume is in veins
Venous Return
- Venous pressure is driving force for return of blood to the heart.
- End diastolic volume (EDV), diastolic volume (DV), stroke volume (SV), and cardiac output (CO) are factors which affect venous return
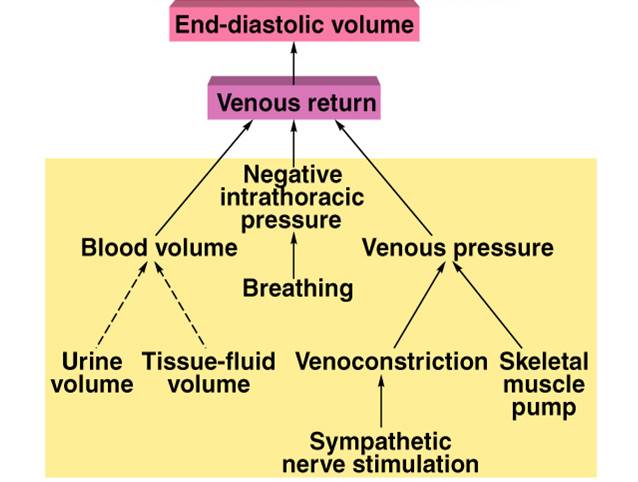
|
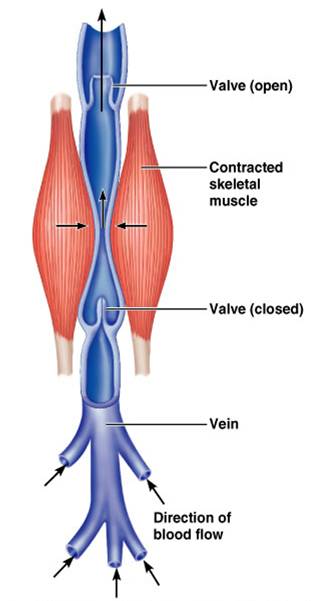
- Venous BP alone is too low to promote adequate blood return and is aided by the:
- Respiratory “pump” – pressure changes created during breathing squeeze local veins
- Muscular “pump” – contraction of skeletal muscles push blood toward the heart
- Valves prevent backflow during venous return
|
 |
Capillaries
Exchange of gases, nutrients, and wastes occurs at the capillaries.
There are 3 major types of capillaries
1. Continuous Capillaries
- Have a continuous lining and are connected by tight junctions
- Have small gaps or clefts between the endothelial cells (large enough to allow limited passage of fluids and small solutes)
- Most common
- Are abundant in skin and muscles, thymus, lungs, and the CNS
2. Fenestrated Capillaries
- Have holes (fenestrations) within each endothelial cell
- The basement membrane is continuous
- Have more permeability to fluids and small solutes than the continuous capillaries
- Are found in small intestine, endocrine glands, kidneys, and ciliary process of the eye
3. Sinusoids
- Have larger gaps than fenestrated capillaries.
- The basement membrane is either discontinuous or absent
- Have large clefts and fenestrations
- Allow large molecules (proteins) and even blood cells to pass out of the vessel
- Blood moves sluggishly through sinusoids allowing blood to be processed and modified
- Are found in liver, bone marrow, lymphoid tissues, some endocrine glands
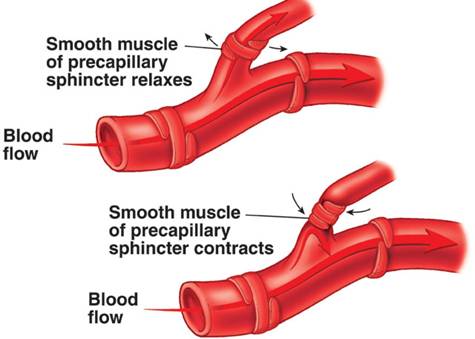
Capillary Beds
Capillaries form networks called capillary beds. Most beds consist of 2 types of vessels:
1. Shunt Capillary (“straight shot” capillary)
2. True Capillaries (these are the actual exchange vessels); number 10-100
A cuff of smooth muscle called a precapillary sphincter acts as a valve to regulate the flow of blood into the capillary bed. Blood flowing into a bed may take 2 routes – through the shunt or through the true
capillaries.
Blood flows from arterioles through metarterioles, then through capillary network
Venules drain the capillaries
Smooth muscle in arterioles, metarterioles, and precapillary sphincters regulate blood flow
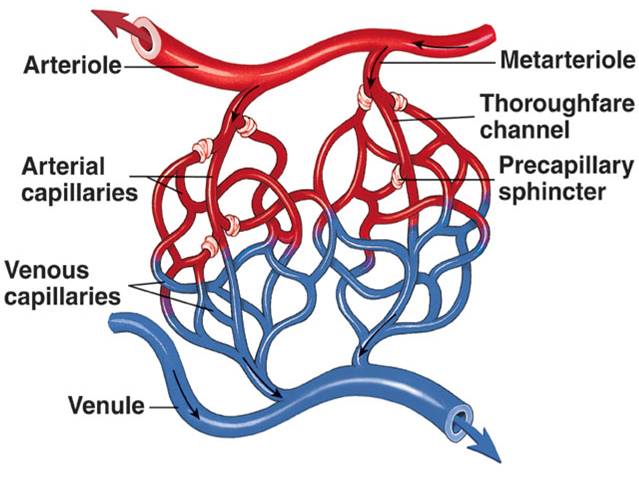
Atriovenous Anastomosis
This is a vascular shunt that directly connects an arteriole to a venule
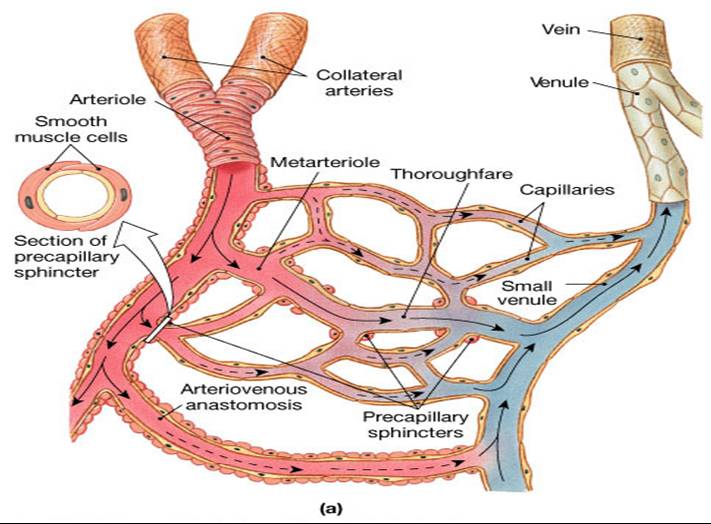
|
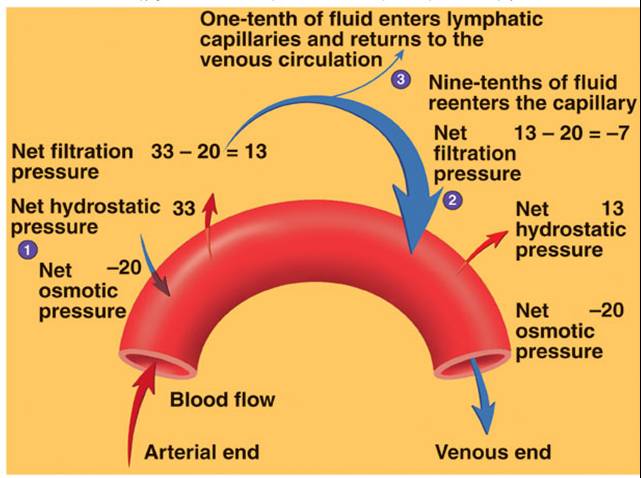
Exchange of Fluid between Capillaries and Tissues
- Hydrostatic pressure, capillary permeability, and osmosis affect movement of fluid into and out of capillaries
- A net movement of fluid occurs from blood into tissues – bulk flow
- Distribution of extracellular fluid (ECF) between plasma and interstitial compartments
- Is in state of dynamic equilibrium.
- Is a balance between pressures in the tissue fluid and blood plasma
- Hydrostatic Pressure:
- Is the pressure exerted against the inner capillary wall
- Promotes formation of tissue fluid
- Across a capillary bed, the hydrostatic pressure quickly drops as blood oves from the higher pressure arteriole end to the lower pressure venule end
- Net filtration pressure
- Colloid osmotic pressure:
- This is the pressure exerted by plasma proteins
- Promotes fluid reabsorption into circulatory system
- Is constant across the capillary bed because the concentration of nonpenetrating solutes does not change from one of the capillary bed to the other
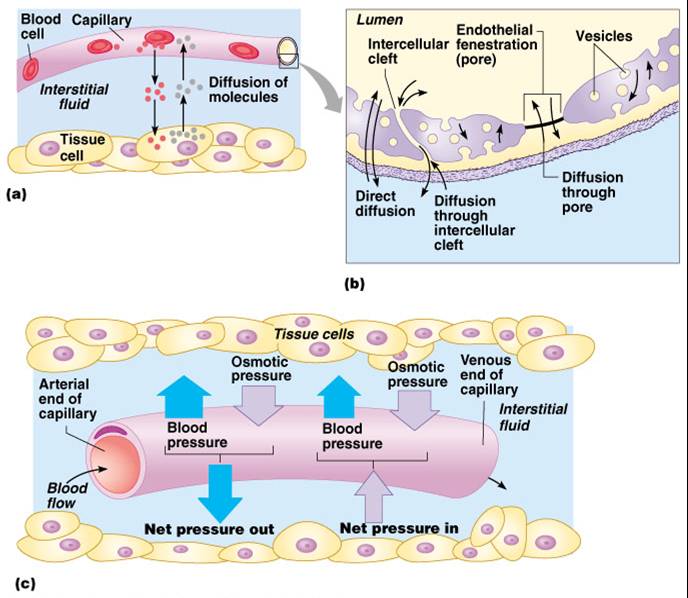
|
Fluid Movement
Starling Force = ( Pc + Pi) - (Pi+ Pp)
Pc = Hydrostatic pressure in the capillary
Pi = Colloid osmotic pressure of the interstitial fluid
Pi = Hydrostatic pressure in the the interstitial fluid
Pp = Colloid osmotic pressure of the blood plasma.
|
|
Lymphatic System
 Click here for an animation that provides an overview of the lymphatic system. Click here for an animation that provides an overview of the lymphatic system.
The cardiovascular system has a close relationship with the lymphatic system
- Is an extensive network of one-way vessels
- Provides accessory route by which fluid can be returned from tissues to the blood
- Lymph is interstitial fluid that enters a lymphatic vessel
- Lymph vessels
- Formed from convergence of terminal lymph vessels (initial lymphatics)
- Eventually empty into the subclavian veins near where blood enters right atrium
- One way valves spaced at intervals direct flow of lymph toward venous outlet in chest
Functions of the Lymphatic System
- Return of excess filtered fluid
- Defense against disease
- Lymph nodes have phagocytes which destroy bacteria filtered from interstitial fluid
- Transport of absorbed fat
- Return of filtered protein
Intrinsic Regulation of Blood Flow (Autoregulation)
- Blood flow can increase 7-8 times as a result of vasodilation of metarterioles and precapillary sphincters
- Response to increased rate of metabolism
- Intrinsic receptors sense chemical changes in environment
- Vasodilator substances produced as metabolism increases
- Decreased 02:
- Increased C02:
- Decreased pH - Lactic acid.
- Increased adenosine/K+ from tissue cells
- Myogenic control mechanism:
Occurs because of the stretch of the vascular smooth muscle - maintains adequate flow.
- A decrease in systemic arterial pressure causes vessels to dilate.
- A increase in systemic arterial pressure causes vessels to contract
Endothelium secretions:
- Nitric Oxide (NO) causes vasodilation
- NO diffuses into smooth muscle:
- Activates cGMP (2nd messenger).
- Endothelin-1 causes vasoconstriction
- Histamine release
- Heat/cold application
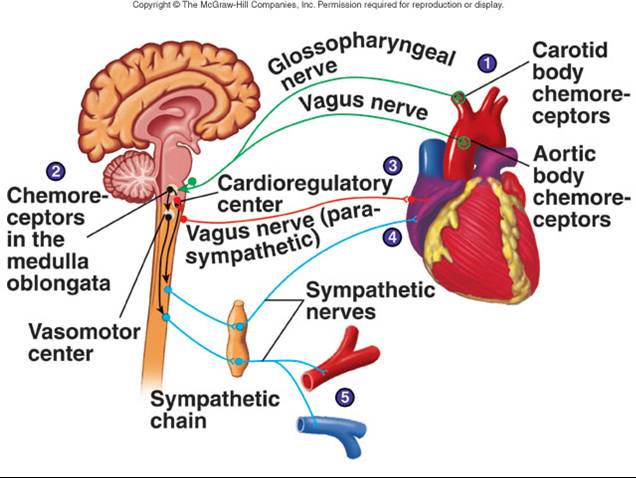
Extrinsic Regulation of Blood Flow
- Sympathoadrenal
- Increase cardiac output
- Increase TPR: Alpha-adrenergic stimulation - vasoconstriction of arteries in skin and viscera
- Parasympathetic
- Parasympathetic innervation limited, less important than sympathetic nervous system in control of TPR.
- Parasympathetic endings in arterioles promote vasodilation to the digestive tract, external genitalia, and salivary glands
Blood Pressure Regulation
Pressure of arterial blood is regulated by blood volume, TPR, and cardiac rate.
- Arteriole resistance is greatest because they have the smallest diameter.
- Capillary BP is reduced because of the total cross-sectional area.
- 3 most important variables are HR, SV, and TPR.
- Increase in each of these will result in an increase in BP.
- BP can be regulated by:
- Kidney and sympathoadrenal system
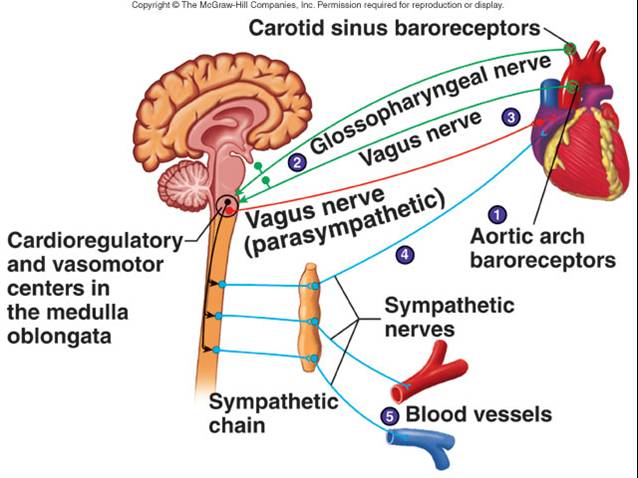
Short-Term Regulation of Blood Pressure
- Baroreceptor Reflexes
- Baroreceptors are sensory receptors that detect changes in blood pressure
- Baroreceptors are located in the carotid sinus, aortic arch, and other arteries
- Changes in peripheral resistance, heart rate, and stroke volume occur in response to changes in blood pressure
 Click here for an animation that reviews baroreceptor reflexes. Click here for an animation that reviews baroreceptor reflexes.
- Chemoreceptor Reflexes
- Chemoreceptors are sensory receptors sensitive to oxygen, carbon dioxide, and pH levels of blood
 Click here for an animation that reviews chemoreceptor reflexes. Click here for an animation that reviews chemoreceptor reflexes.
- Central Nervous System Ischemic Response
(CNS)
- Results from high carbon dioxide or low pH levels in medulla and increases peripheral resistance
Long-Term Regulation of Blood Pressure
- There are 5 mechanisms by which blood pressure is regulated over the long term:
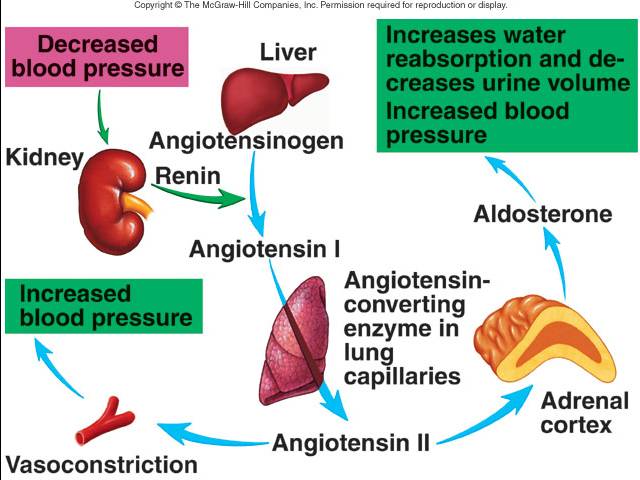
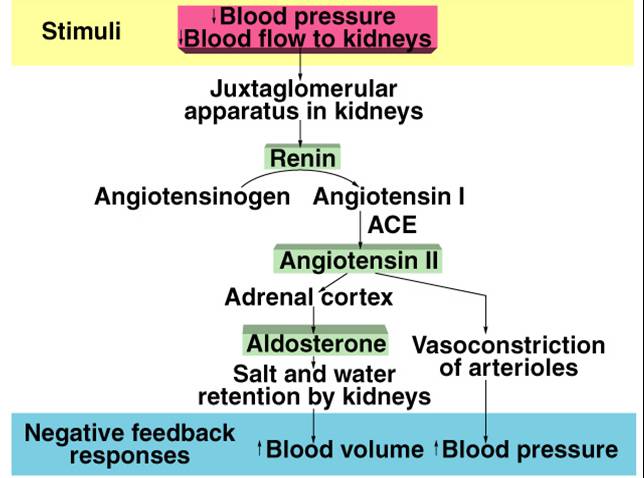
1. Renin-Angiotensin-Aldosterone Mechanism
This mechanism detects a fall in blood pressure and initiates a series of events that help to bring blood pressure back to normal. For details on the RAA mechanism, click here.
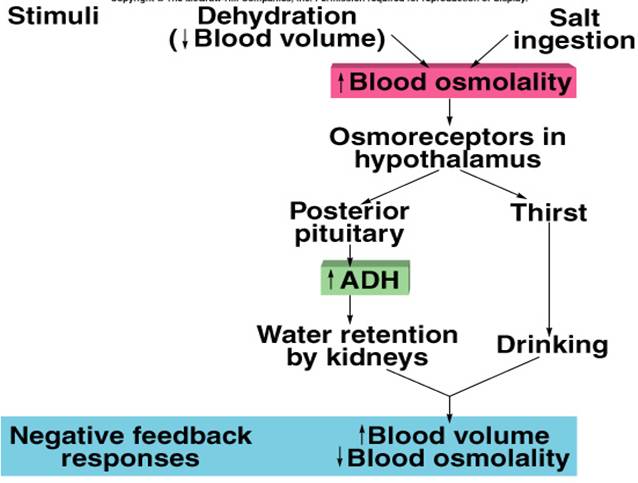
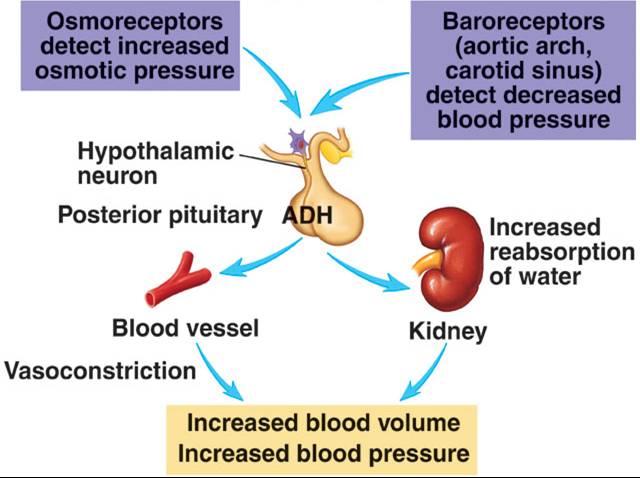
2. Antidiuretic Hormone (ADH or Vasopressin) Mechanism
- ADH is released by the posterior pituitary when osmoreceptors in hypothalamus detect an increase in plasma osmolality
- Dehydration or excess salt intake:
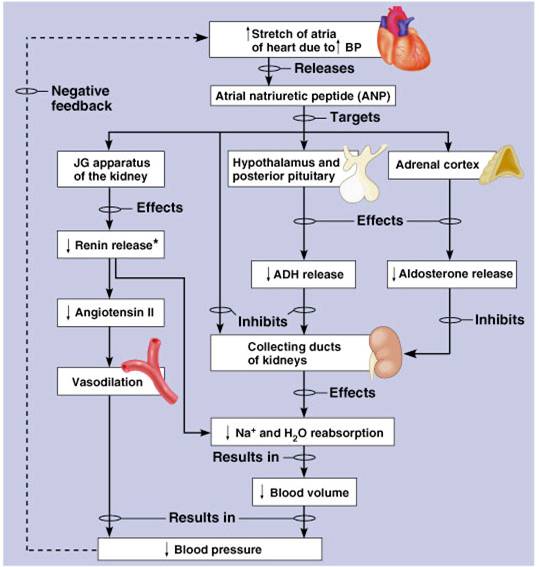
3. Atrial Natriuretic Peptide Mechanism
- Produced by the atria of the heart in response to increased blood pressure
- Stretch of atria stimulates production of ANP.
- Antagonistic to aldosterone and angiotensin II.
- Promotes sodium and water excretion in the urine by the kidney.
- Promotes vasodilation
4. Fluid Shift Mechanism
5. Epinephrine/Norepinephrine Mechanism
- Are produced by cells in the adrenal medulla in response to emergency or stressful situations
- These hormones increase heart rate and blood vessel constriction, result in an increase in blood pressure
Regulation of Blood Pressure by ADH (Vasopressin)
Regulation of Blood Pressure by Atrial Natriuretic Peptide (ANP)
Cerebral Circulation
Cerebral blood flow is not normally influenced by sympathetic nerve activity.
Normal range of arterial pressures:
Cerebral blood flow regulated almost exclusively by intrinsic mechanisms:
- Myogenic:
- Dilate in response to decreased pressure.
- Cerebral arteries also sensitive to [C02].
- Dilate due to decreased pH of cerebrospinal fluid.
- Metabolic:
- Sensitive to changes in metabolic activity.
- Areas of brain with high metabolic activity receive most blood.
- May be caused by [K+].
- controlled by autonomic nervous system and endocrine system.
Sympathoadrenal:
Increase CO, Increase TPR
- NE + a1 adrenergic stimulation: vasoconstriction of arteries in skin and viscera.
- EPI + b1 receptors increase SV
- Cholinergic sympathetic fibers - vasodilate vessels of skeletal muscles.
Parasympathetic nervous system innervation limited, Promotes vasodilation to the digestive tract, external genitalia, and salivary glands. Less important than sympathetic nervous system in control of TPR. Parasympathetic endings in arterioles promote vasodilation.
Top ...... Main Page
|